Parkinson’s comes on slowly, and diagnosing the often-devastating movement disorder, particularly in its early stages, usually entails having patients perform a variety of mobility tasks, observing their walking and movement patterns, and testing their reflexes. In all, it’s a time-consuming and labor-intensive process for both clinicians and patients.
Researchers in the University of Maryland, College Park’s Center for Bioinformatics and Computational Biology (CBCB) have just published research that may soon make a diagnosis easier on everyone involved.
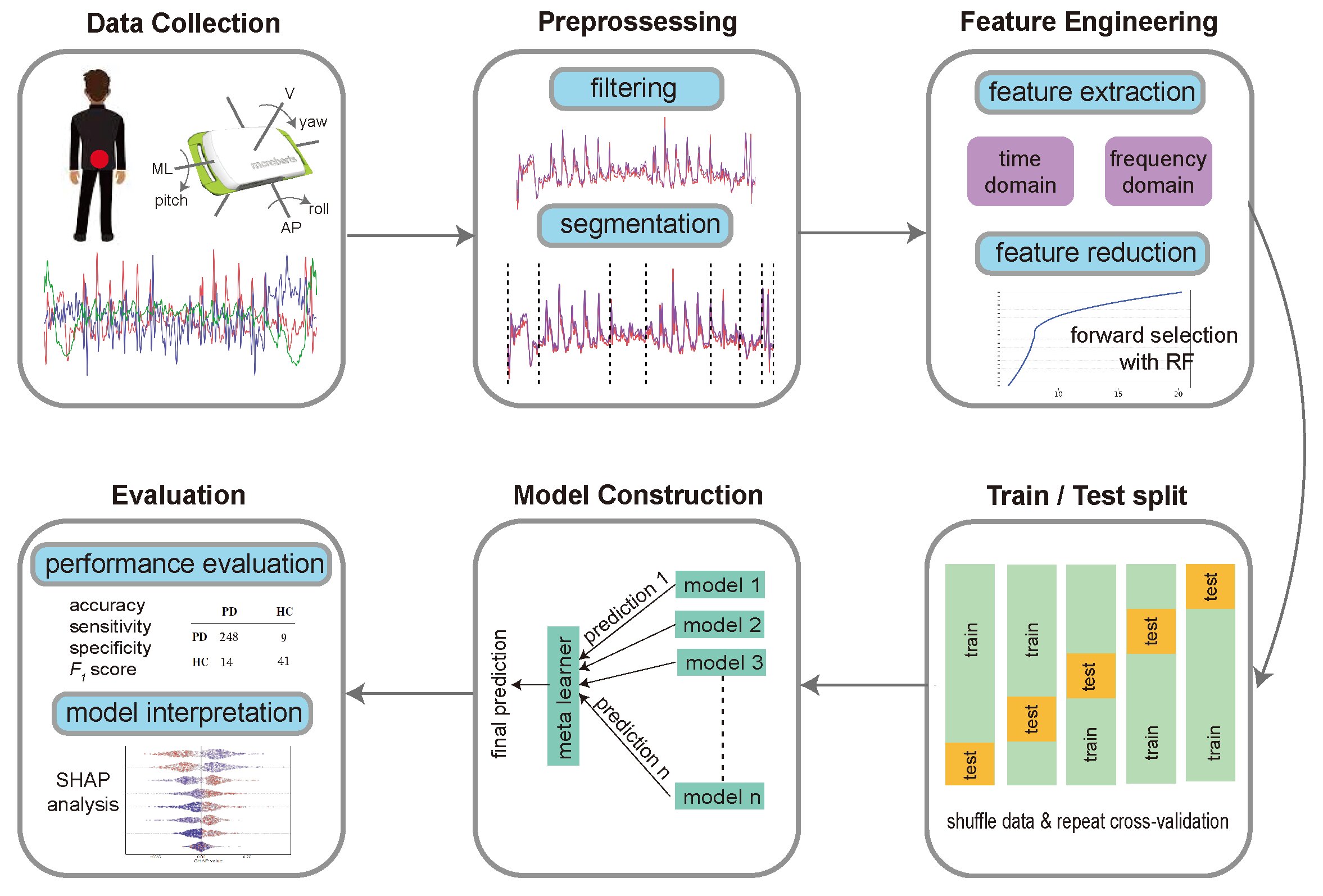
They’re working with colleagues at the University of Maryland, Baltimore and elsewhere to use machine learning algorithms to analyze data from wearable, movement-tracking sensors to help automate parts of the process. Ultimately, the researchers say, this can lead to more accurate and earlier diagnoses, which in turn can lead to earlier therapeutic interventions.
Rana Khalil, a sixth-year Ph.D. student in computer science at UMD and lead author of a new paper detailing the research published in the journal Sensors, worked on the project with her adviser, Michael Cummings, a professor of biology and director of CBCB.
Parkinson’s disease starts with mild symptoms, such as a subtle tremor in one hand, but may progress to severe muscle rigidity and an inability to walk without help. According to the National Institutes of Health, approximately 500,000 people in the U.S. have been diagnosed with Parkinson’s. But because many people are undiagnosed—or have been misdiagnosed—experts believe that as many as one million Americans may have the debilitating disease.
This considerable discrepancy highlights one of the central problems faced by clinicians and patients: the challenge of accurately diagnosing the disease. “The diagnosis of mobility disorders is very difficult,” said Cummings, who has an appointment in the University of Maryland Institute for Advanced Computer Studies (UMIACS). “Much of the process is subjective, and as such, isn’t highly accurate.”
A more precise means of diagnosis could help alleviate the physical and psychological distress patients face by cutting down on multiple clinic visits and misdiagnoses, he said.
Although wearable sensors to diagnose Parkinson’s have been developed in the past, their complexity has prevented doctors from using them in clinics. The new research simplifies the use of sensors and machine learning in a clinical setting, Cummings said.
It demonstrated that a single sensor placed on the lower back and a single mobility task involving multiple movements can effectively distinguish individuals with Parkinson’s disease from controls. The researchers then developed a sophisticated machine learning framework that analyzed patterns and variations in the data.
This enhanced the identification of disease symptoms and diagnostic accuracy, with the study reporting an accuracy of 92.6% in identifying participants across different Parkinson’s stages, surpassing the accuracy of 81% previously reported for clinical diagnosis by movement disorder experts.
Moving forward, CBCB researchers are already deeply involved in a related study on distinguishing Parkinson’s from other movement disorders, attempting to further enhance accuracy and deter misdiagnosis.
More information:
Rana M. Khalil et al, Simplification of Mobility Tests and Data Processing to Increase Applicability of Wearable Sensors as Diagnostic Tools for Parkinson’s Disease, Sensors (2024). DOI: 10.3390/s24154983
Citation:
Wearable sensors, machine learning system could pinpoint Parkinson’s (2024, September 23)
retrieved 5 October 2024
from https://medicalxpress.com/news/2024-09-wearable-sensors-machine-parkinson.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.