Using artificial intelligence (AI) to aid clinical decision making in identifying and managing myocardial infarction (MI; heart attack) in patients presenting to the emergency department (ED) with suspected cardiac conditions does not improve cardiovascular outcomes. However, this AI-based clinical decision support is safe and increases the adoption of evidence-based care, according to late breaking research presented in a Hot Line Session at this year’s ESC Congress 2024 in London, UK (30 Aug.–2 Sept.).
“A key promise of AI in health care is as a tool to help medical professionals diagnose patients faster and more accurately as well as more objectively quantify prognosis, ultimately allowing them to initiate the appropriate treatment sooner to optimize patient outcomes,” said lead author Kristina Lambrakis at the Victorian Heart Hospital, Monash Health, the Victorian Heart Institute, Monash University and College of Medicine and Public Health, Flinders University Australia.
She added, “Our large cluster-randomized trial involving patients presenting to the ED with suspected cardiac conditions across South Australia did not improve clinical outcomes, however it did highlight the ability of real-time AI to influence clinical decisions and practice towards evidence-based care. Greater adoption of AI insights and integration of AI insights within clinical workflows will likely be required to improve clinical outcomes.”
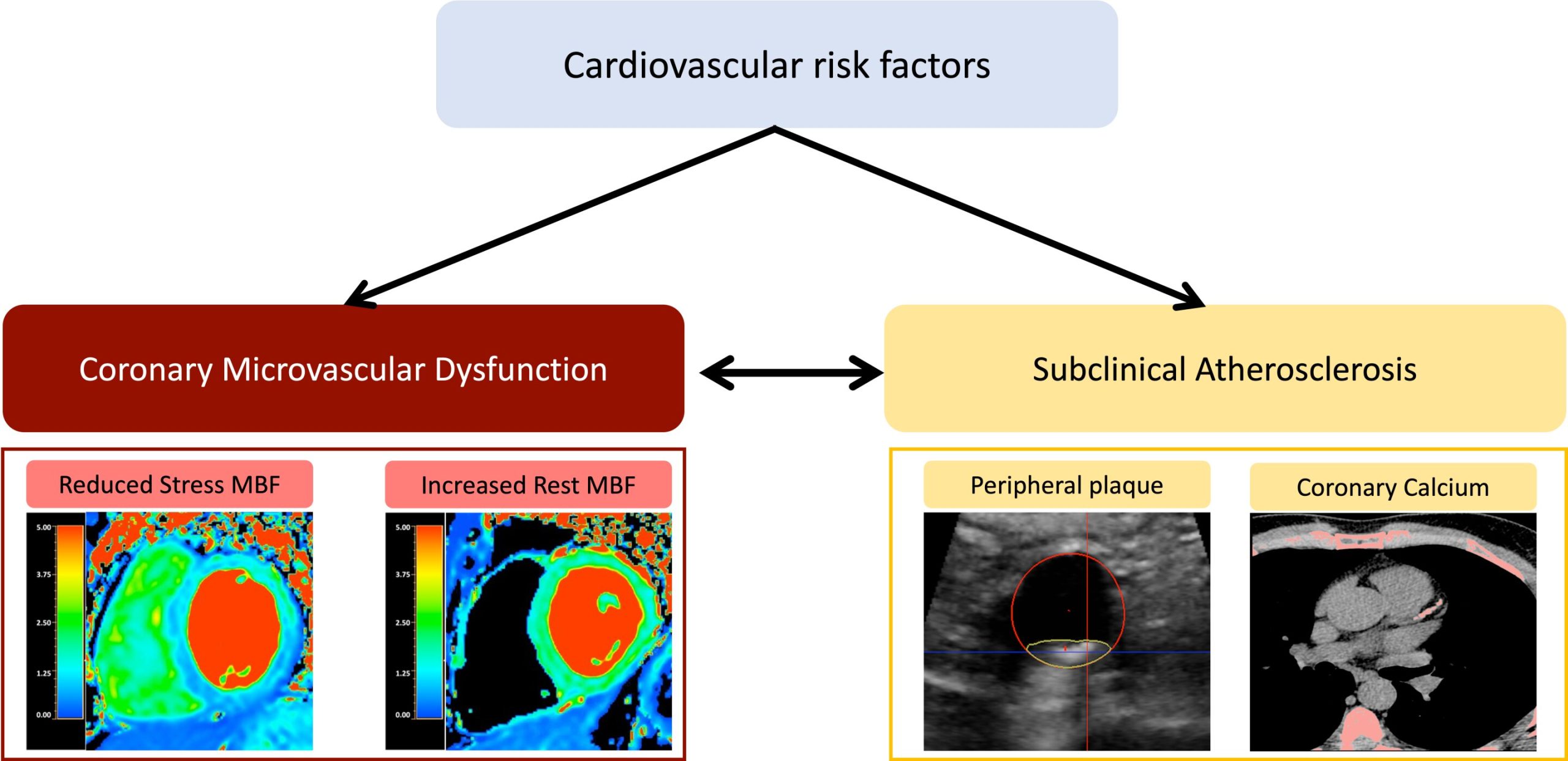
Widespread use of high sensitivity troponin (hs-cTn) tests, a biomarker detected in the blood which indicates heart muscle injury, has increased the ability to identify individuals with even very minor injury to the heart muscle. However, these more sensitive tests have also made the interpretation of troponin results more challenging as elevated results can now be due to a large number of causes other than type 1 MI (heart attack due to coronary plaque rupture), with misinterpretation leading to potentially unwarranted investigation, risk, and costs.
In addition, this complex diagnostic decision-making is frequently required to be made by clinicians in the ED who do not have advanced cardiology training and who see highly undistinguishable patients, making it even more challenging for them to differentiate the various forms of myocardial injury in interpreting hs-cTn results.
To help doctors make the correct diagnosis, the current 2018 Fourth Universal Definition of Myocardial Infarction (UDMI) guidance aims to support hs-cTn interpretation by delineating MI and myocardial injury classifications, which require specific treatments.
The 4th UDMI defines myocardial injury as a troponin elevation where at least one value is above the 99th percentile upper reference limit. The difference in troponin levels between repeated sampling results defines whether it is an acute or chronic myocardial injury. Myocardial injury can be caused by numerous situations including sepsis, kidney disease, heart failure, and strenuous exercise.
To diagnose a myocardial infarction (MI), the patient must have acute myocardial injury as well as evidence of acute myocardial ischemia—oxygen shortage supplying the heart muscle detected by ECG, symptoms such as pain in the chest, arms or jaw, or imaging evidence.
Whether clinical use of the 4th UDMI classification system has resulted in improved patient outcomes is not known. The use of AI algorithms based on the 4th UDMI to support clinical decision making could help guide hs-cTn interpretation and improve outcomes.
To fill this important evidence gap, the RAPIDx AI trial enrolled 14,131 patients (aged 18 and older) presenting to the ED and receiving hs-cTn testing across six metropolitan and six rural EDs across South Australia between April 15 and December 31, 2023. Six hospitals were randomly assigned to the control arm (i.e., unchanged standard of practice) and six to the intervention arm (i.e., implementation of AI-based clinical decision support).
A total of 3,029 patients (average age 74.5 years; 58% female) with myocardial injury (elevated troponin based on hs-cTn) and suspected cardiac cause were included in the primary intention-to-treat analysis (1,461 patients who presented to control hospitals and 1,568 to hospitals with AI decision support).
The main measure of interest was cardiovascular (CV) death, new/recurrent MI, and unplanned CV readmission within 6 months. The safety endpoint was all-cause death or MI within 30 days among those directly discharged from the ED.
In the intention-to-treat analysis, the researchers found no differences in outcomes between the groups, with 408/1568 participants (26.0%) in the intervention group and 385/1461 (26.4%) in the control group experiencing a CV death, MI, or unplanned CV readmission within 6 months.
Similarly, in the entire cohort, the primary end-point occurred in 680 (9.4%) participants in the intervention group and 718 (10.4%) controls.
Importantly, among patients not classified as type 1 MI by AI-driven decision support (i.e. where coronary angiography has not been shown to be of benefit), invasive coronary angiography was 47% less likely to be undertaken in the intervention group compared to the usual care group (66/1265; 5% vs. 112/1186; 9.4%).
Additionally, where patients were classified as having a type 1 MI by the AI-based decision support, they were more likely to be prescribed statins (82% [248/303] vs. 68% [187/275]); more likely to be given antiplatelet therapy (56% [248/303] vs. 44% [120/275]); and more likely to be prescribed a mineralocorticoid inhibitor (56%[78/303] vs. 44% [48/275]) compared to the usual care group.
Among patients directly discharged from the ED, those receiving care in hospitals with the decision support did not die or have an MI within 30 days at a higher rate than those in hospitals who received usual care (0.86% [40/4664] vs. 1.1% [48/4350] non-inferiority p
“We found no increase in early hazards or negative impacts on ED discharge decisions, establishing the safety of AI-based clinical decision support,” said senior author, Professor Derek Chew, at the Victorian Heart Hospital, Monash Health, Victorian Heart Institute, Monash University and College of Medicine and Public Health, Flinders University, Australia.
“Our next steps include exploring approaches to enhancing trust and adoption of AI-based clinical decision support in the clinical community, investigating new models of care within which such AI-based decision support tools could be integrated to drive health system effectiveness and efficiency, and evaluating AI-based decision support for other acute cardiac conditions where early recognition represents a key challenge and driver in optimizing outcomes.”
Citation:
Using AI to support heart attack diagnosis in emergency department does not improve patient outcomes, research finds (2024, September 2)
retrieved 2 September 2024
from https://medicalxpress.com/news/2024-09-ai-heart-diagnosis-emergency-department.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.