Researchers from Weill Cornell Medicine have used a cutting-edge model system to uncover the mechanism by which SARS-CoV-2, the virus that causes COVID-19, induces new cases of diabetes, and worsens complications in people who already have it. The team found that viral exposure activates immune cells that in turn destroy beta cells, the pancreatic cells that produce insulin.
The study is published in Cell Stem Cell.
“There has long been a hypothesis in the field that certain viral infections may trigger type 1 diabetes,” said co-corresponding author Shuibing Chen, director of the Center for Genomic Health, the Kilts Family Professor of Surgery and a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine. “But we were able to show how this happens in the context of COVID-19 infection.”
“When someone has severe COVID-19, of course the first priority is to treat the life-threatening symptoms,” said co-corresponding author Dr. Robert Schwartz, an associate professor of medicine at Weill Cornell Medicine and a gastroenterologist and hepatologist at NewYork-Presbyterian/Weill Cornell Medical Center. “But moving forward, there may be a way to develop clinical therapeutics that help avoid later injury to organs like the pancreas.”
Dr. Liuliu Yang and Dr. Yuling Han, who were postdoctoral fellows in the Department of Surgery at the time of the study, and Dr. Tuo Zhang, an instructor in microbiology and immunology at Weill Cornell Medicine, were co-first authors of the paper.
From the early days of the COVID-19 pandemic, doctors caring for sick patients observed that the virus affected a number of organ systems, including not only the lungs but also the heart, liver, colon and pancreas. For the current work, the researchers started with samples of pancreatic tissue from autopsies of people who had died of COVID-19. They observed that the pancreatic islets, the parts of the pancreas that generate the insulin to regulate blood sugar, were damaged.
They then used an analysis technique called GeoMx to study the samples in more detail. This revealed the presence of immune cells called proinflammatory macrophages in the tissues. The job of these macrophages is to kill off pathogens, but they sometimes cause collateral damage to healthy tissues.
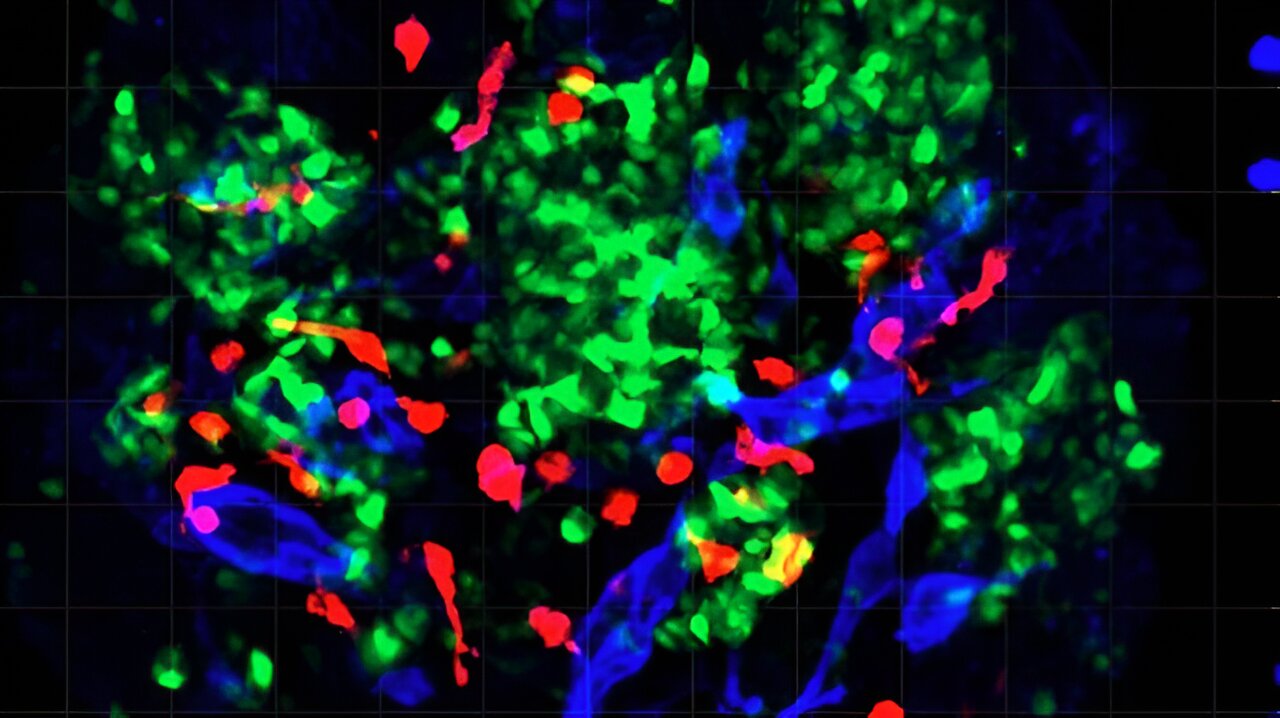
To learn more about this activity, the team used a model system developed in the Chen Lab that has never been used before; pancreatic islet organoids (mini organs) that included both a vascular system and immune cells.
“If we want to use organoids to study how a disease progresses, it’s important to be able to include components of the immune system in these models,” said Chen. In this case, after infecting the organoids with SARS-CoV-2, they found the macrophages appeared to be killing off the beta cells through a type of cell death called pyroptosis.
The team also used the organoids to study how the pancreas responds to infection with another infectious virus: coxsackievirus B4, which has been implicated in the onset of type 1 diabetes. They found a similar macrophage response.
“Moving forward, this organoid system is going to be useful for looking at other viruses as well,” Schwartz said.
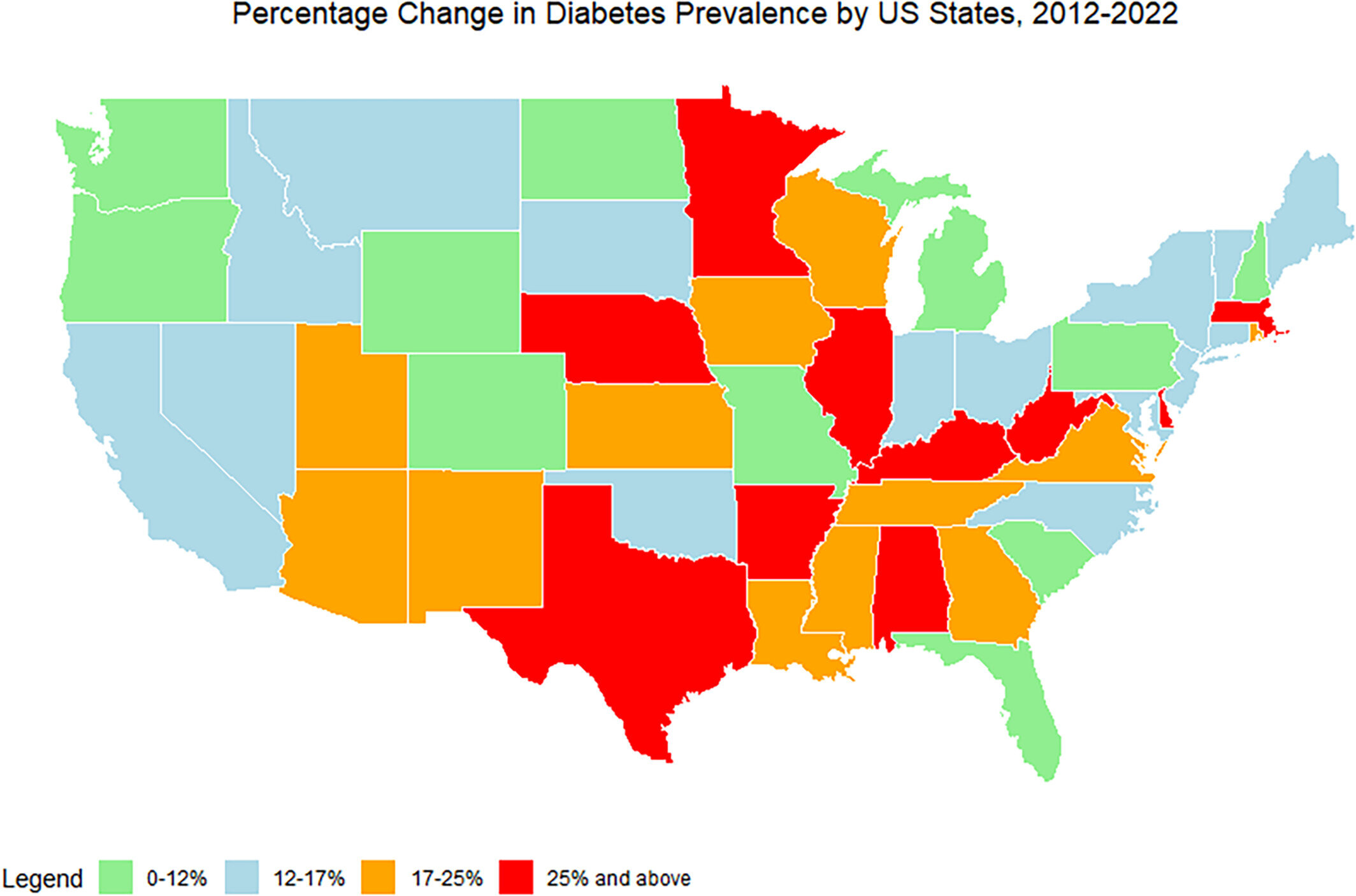
Further research on the signaling molecules that activate the macrophages also suggested potential interventions for protecting beta cells from damage in patients with severe infections. Although it is too early to begin testing any treatments, this is something that may be possible in the future. This work could also help shed light on the underlying causes of long COVID, a condition that is believed to affect more than 15 million people in the United States.
More information:
Liuliu Yang et al, Human vascularized macrophage-islet organoids to model immune-mediated pancreatic β cell pyroptosis upon viral infection, Cell Stem Cell (2024). DOI: 10.1016/j.stem.2024.08.007
Citation:
Study reveals how COVID-19 infection can cause or worsen diabetes (2024, September 16)
retrieved 21 September 2024
from https://medicalxpress.com/news/2024-09-reveals-covid-infection-worsen-diabetes.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.