The accumulation of fats in the liver is driven by high-fat diets and obesity, and is becoming an increasingly prevalent global health concern. Characterized by excessive fat accumulation in the liver, this condition poses significant risks for various metabolic disorders.
While much of the existing research has focused on fat metabolism within the liver itself, emerging findings emphasize the critical role of the gut in this complex process.
Proglucagon-derived peptides (PGDPs), including glucagon, GLP-1, and GLP-2, are known to be the key hormones that regulate lipid metabolism in the liver. Derived from the same precursor—proglucagon, previous studies have shown that both GLP-1 and GLP-2 are involved in lipid accumulation indirectly in the liver. However, their specific contributions to liver fat accumulation are not yet fully understood.
A recent study, led by Associate Professor Yusuke Seino from Fujita Health University and published in Nutrients on 14 July 2024, explores how PGDPs impact fat absorption and liver fat buildup.
The team of researchers included lead researchers Mr. Koki Nishida, Mr. Atsushi Suzuki, and Mr. Yoshiki Hirooka from Fujita Health University, along with Mr. Yoshikata Hayashi from Nagoya University.
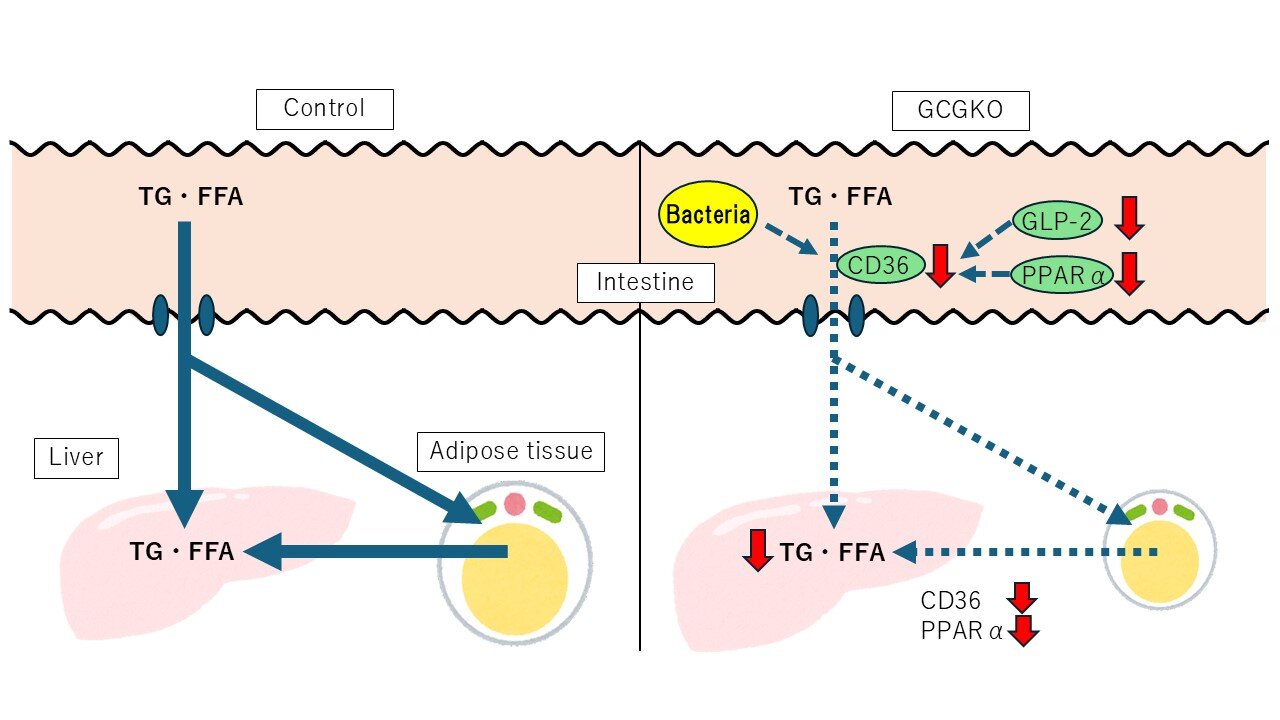
Using genetically modified mice lacking PGDPs (GCGKO mice), the study investigates the response of mice to a high-fat diet (HFD) for seven days and sheds light on a potential new strategy for preventing fatty liver.
“When we subjected both GCGKO mice and control mice to an HFD for one week, the GCGKO mice exhibited a significantly lower increase in hepatic free fatty acid (FFA) and triglyceride levels, along with reduced adipose tissue weight,” says Dr. Seino.
These effects were attributed to a decrease in lipid absorption via the CD36 pathway in the intestinal tract, despite a reduced fat-burning capacity (β-oxidation) in the liver.
Additionally, the study found lower expression levels of genes involved in FFA oxidation in HFD-fed GCGKO mice. Particularly, Pparα (peroxisome proliferator receptor alpha) and Cd36 (cluster of differentiation 36) mRNA levels were reduced in the duodenum, correlating with a decrease in fat uptake in the intestines and increased fecal cholesterol content.
This suggests that the absence of PGDPs prevents diet-induced fatty liver by lowering intestinal fat absorption.
Notably, the researchers found that despite lower fat-burning activity in the liver, the primary factor preventing fat accumulation was reduced fat absorption from the intestines. HFD-fed GCGKO mice also showed lower plasma triglyceride levels during the oral fat tolerance test (OFTT), further confirming reduced lipid absorption.
Moreover, the study underscores the intricate relationship between diet, hormonal responses, and intestinal microbiota. The HFD-fed GCGKO mice demonstrated notable shifts in gut bacteria, with an increase in Parabacteroides and a decrease in Lactobacillus, both linked to obesity resistance. These changes further point to the possibility of dietary and hormonal interventions to enhance gut health and metabolic function.
Adding further, Dr. Seino notes, “If we can examine in more detail how PGDPs specifically regulate lipid absorption in the gut, we hope to clarify the relationship between diet, hormones, and intestinal bacteria sufficiently to recommend a diet that is less conducive to obesity and fatty liver disease.”
Talking about the long-term implications of their research, Dr. Seino says, “In the future, oral dual antagonists of GLP-2 and glucagon could emerge as potential therapies for obesity and fatty liver, especially given their roles in insulin sensitivity and lipid metabolism.”
In summary, these findings pave the way for the development of targeted therapies aimed at combating this growing health problem, potentially improving outcomes for millions of people affected by fatty liver disease worldwide.
More information:
Koki Nishida et al, Impaired Fat Absorption from Intestinal Tract in High-Fat Diet Fed Male Mice Deficient in Proglucagon-Derived Peptides, Nutrients (2024). DOI: 10.3390/nu16142270
Citation:
Study reveals crucial role of intestinal absorption in preventing dietary-induced fatty liver disease (2024, October 7)
retrieved 8 October 2024
from https://medicalxpress.com/news/2024-10-reveals-crucial-role-intestinal-absorption.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.