Patient-derived parathyroid organoids (PTOs) could pave the way for future physiology studies and drug-screening applications, as shown in a study published on October 27 in the journal Stem Cell Reports.
“We are the first group in the world that was able to isolate parathyroid stem cells and maintain these cells in our lab as organoids for an extended period of time,” says co-senior study author Schelto Kruijff of the University Medical Center Groningen. “Our research introduces the PTO as a new model for research on parathyroid diseases.”
Parathyroid diseases are characterized by alterations in the excretion of parathyroid hormone, leading to abnormal blood calcium concentrations. The development of parathyroid-targeted treatments and imaging tracers could benefit from in vitro models. Organoids are 3D structures that closely recapitulate tissue architecture and cellular composition and are developed from stem cells. These models have proven very useful for studying tumor behavior and assessing drug responses and have provided a platform for long-term in vitro experimentation.
“We have shown that the parathyroid gland contains stem cells that are able to produce organoids. These organoids mimic the patient condition, are able to produce hormone, express specific markers, and show comparable reactions to drugs,” says Kruijff.
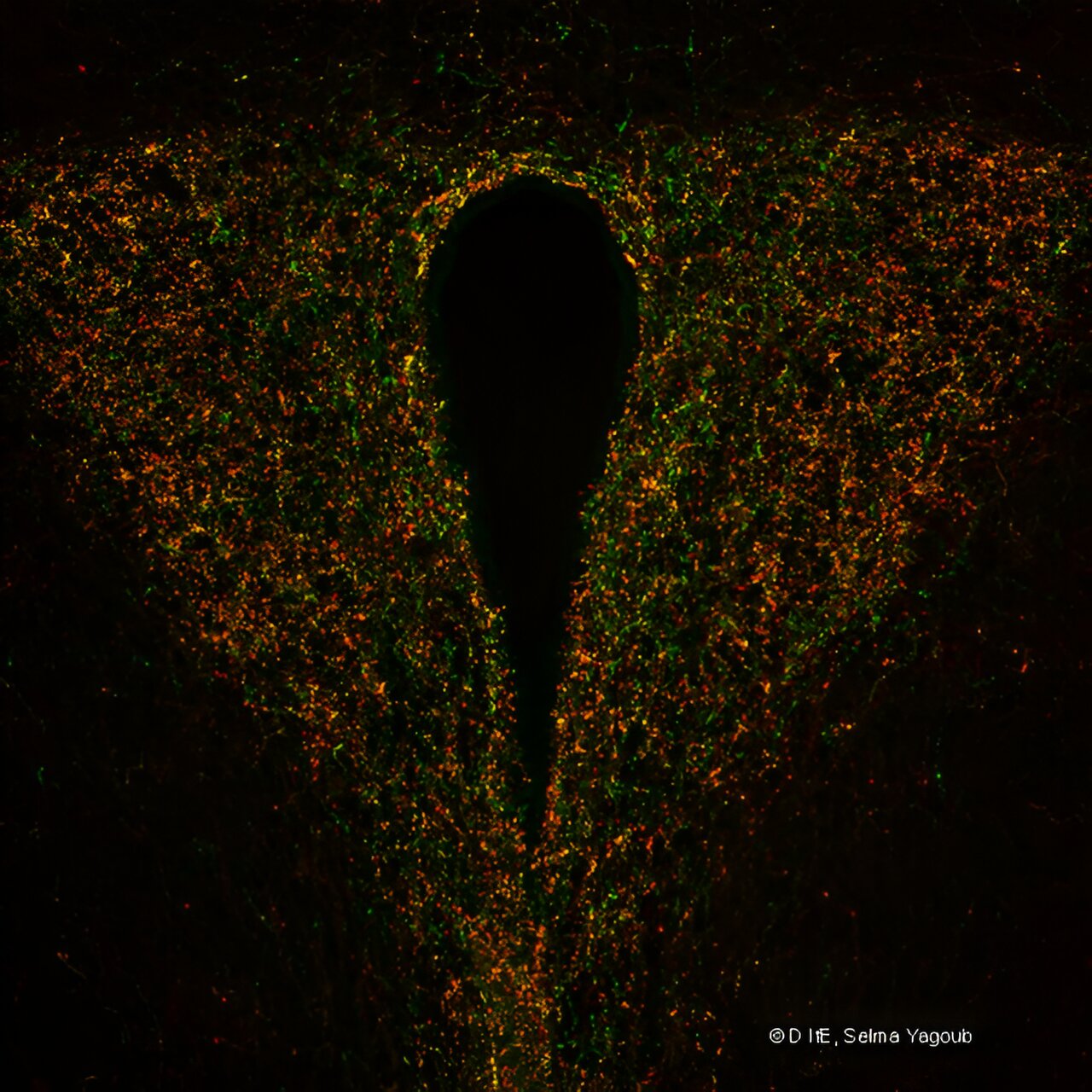
In this study, Kruijff and co-senior study author Rob Coppes of the University Medical Center Groningen set out to establish a patient-derived PTO model representing human parathyroid tissue. The researchers obtained human benign hyperplastic parathyroid tissue from patients undergoing parathyroid surgery. They isolated parathyroid stem cells from the tissue and examined their potential to expand and form PTOs.
The PTOs resembled the original tissue on both gene and protein expression levels and functionality. Additional results demonstrated increased and decreased hormone secretion in response to changes in calcium concentration and parathyroid hormone-lowering drugs. Moreover, the researchers found specific parathyroid-targeted tracer uptake in the PTOs. Taken together, the results demonstrate that these organoids could model human parathyroid functionality.
One study limitation was the absence of the original microenvironment, including blood vessels and fluctuating concentrations of extracellular signals. Nonetheless, the functional testing and tracer experiment showed that the PTOs are a highly suitable model that resembles functional parathyroid tissue.
In future studies, the researchers are planning to transplant these organoids in rats with hypoparathyroidism to study their function in a living animal model. “These organoids can be used to test future parathyroid-targeted drugs and imaging tracers. When using organoids, less animal testing needs to be performed,” Kruijff says. “Also, this technique could be used to try to culture healthy parathyroid gland organoids in order to treat patients with hypoparathyroidism.”