Health care is a leading contributor to the world’s carbon footprint. New analysis on the environmental impact of two common heart procedures shows it is possible to make changes within cardiac care, without compromising on quality of health care.
A team of researchers at the University of Sydney, including a sustainability analyst, a sociologist and cardiologist, has been able to map the carbon footprint of a cardiac patient, from hospital admission to discharge.
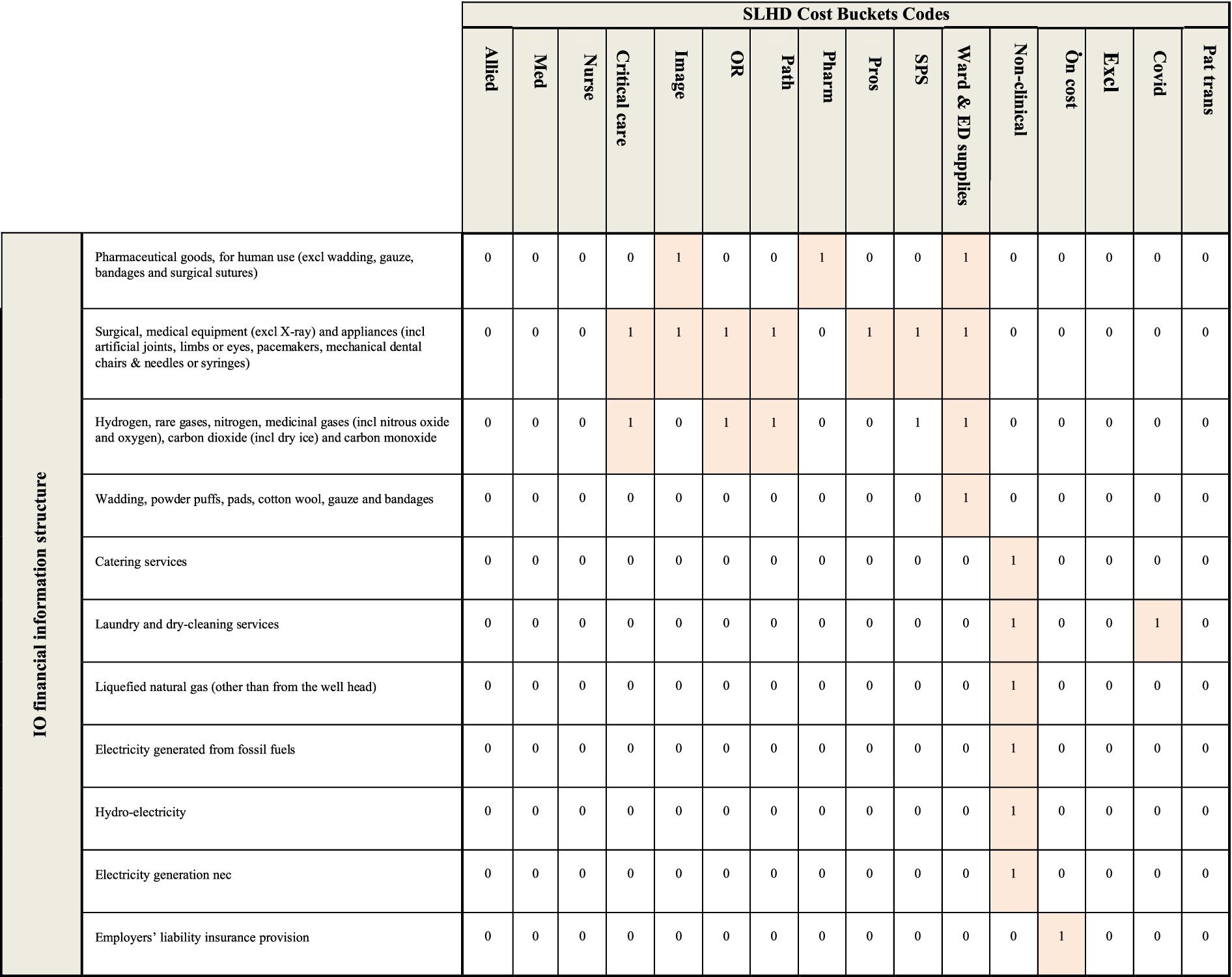
The study found that in Australia, the carbon footprint of a patient with two blocked heart vessels going to hospital for elective open-heart surgery was 4.9 times greater than a patient receiving a coronary stent (a tube used to keep open a blood vessel).
This is the first time researchers have been able to compare the carbon footprints of two clinical procedures that included the patient’s entire stay at a hospital.
“The aim is never to compromise quality of care; but to introduce carbon emissions as one of the possible considerations in decision making, especially as this issue becomes more relevant to everyone’s health,” said senior author Professor David Celermajer, from the Sydney Medical School, and Charles Perkins Centre.
The analysis in Frontiers of Public Health uses a mathematical method known as EEIO (environmentally extended input output) analysis, that paints a more systemic picture of health care’s carbon footprint than previously available. This was because it treats a patient’s stay as not isolated to the immediate impacts of a single medical procedure and considers the full supply-chain impact of the patient’s stay in hospital.
The calculation considered the intricate systems behind health care, including the greenhouse gases emitted to support each step of the patient’s stay at the hospital. This included greenhouse gases produced to conduct medical tests, manufacturing and delivering surgical equipment and supplies, as well as disposing of the resulting waste.
The researchers say EEIO is a valuable tool to help map carbon footprints in health care for other medical fields, not just cardiology.
“The results offer a unique and more complete picture of the full climate change impact of health care,” said the study’s first author Dr. Fabian Sack from the Sydney Environment Institute and the Centre for Integrated Sustainability Analysis, in the School of Physics.
“Health care contributes to seven percent of Australia’s total carbon footprint. The study shows medical professionals that, armed with the right data, we can keep both patient and planet in mind when it comes to clinical decisions and health care administration, and without compromising standards of care,” he said.
Professor David Celermajer , who is also from Royal Prince Alfred Hospital said, “Clinical decision making is complex and is driven mainly by the likely medical outcomes, as discussed between patients, their families and their doctors.
“We hope that our findings will influence patients and doctors to also consider carbon emissions, as a part of their decision-making processes—especially where two alternative treatment choices may have quite similar medical outcomes.
Deputy Director of the Sydney Environment Institute, Professor Danielle Celermajer, said, “This landmark study provides a crucial proof of concept—that the method we used can offer medical professionals and policymakers alike a holistic picture of the environmental impact of health care.
“As the impacts of fossil fuel emissions on all aspects of life, including on human health, become ever greater, communities are going to have to take seriously the contributions that all industries make to those emissions. How and to what extent we factor in emissions profiles into institutional design and decision making are critical questions that lie before us; but we cannot begin to answer them without the data,” she said.
“This research is pointing to how we can more efficiently and effectively collect that data.”
More information:
Fabian Sack et al, Healthcare-related carbon footprinting—lower impact of a coronary stenting compared to a coronary surgery pathway, Frontiers in Public Health (2024). DOI: 10.3389/fpubh.2024.1386826
Citation:
Researchers map carbon footprint of cardiac patients, from hospital admission to discharge (2024, September 2)
retrieved 2 September 2024
from https://medicalxpress.com/news/2024-09-carbon-footprint-cardiac-patients-hospital.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.