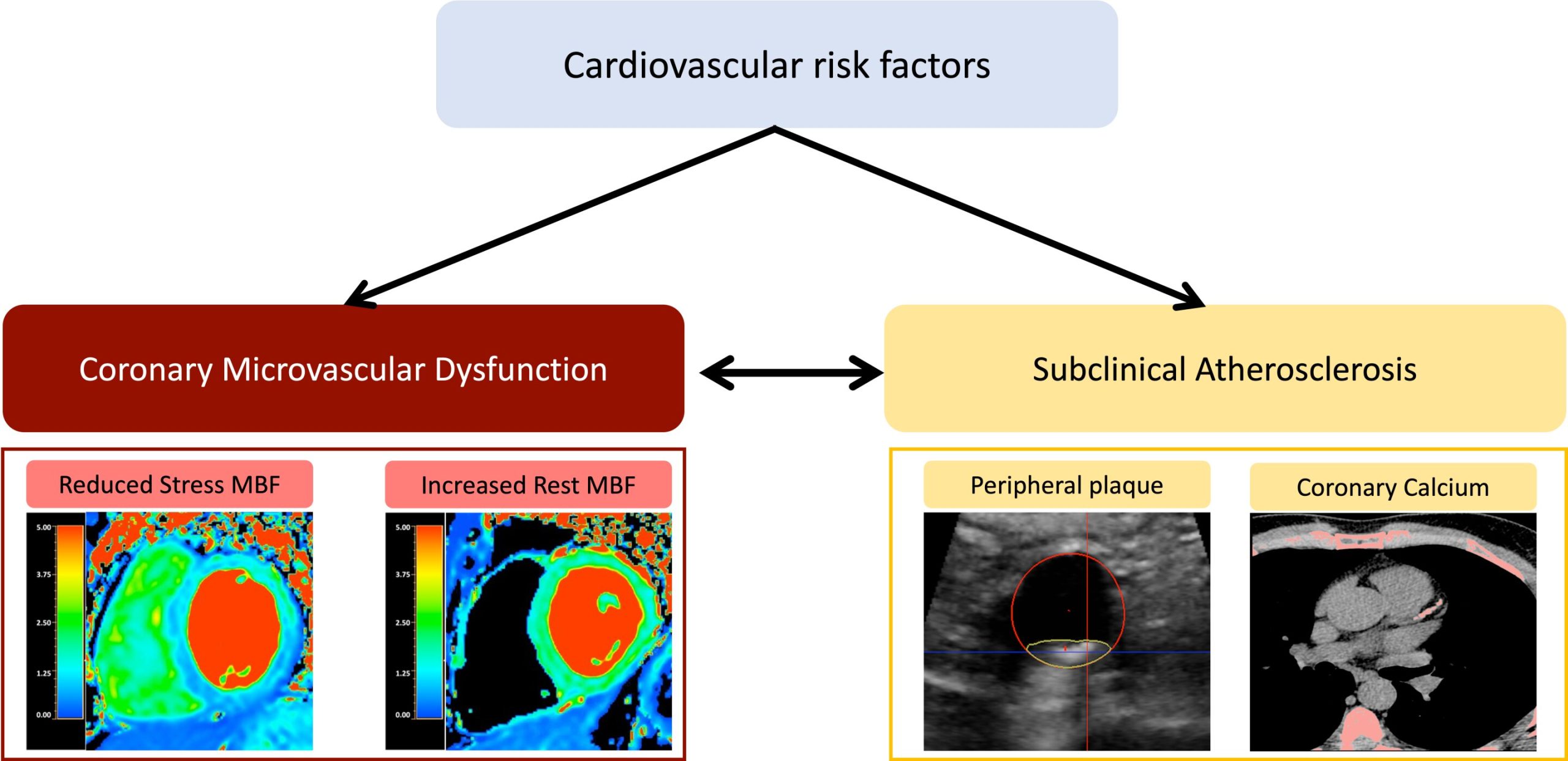
Variants in a gene that plays a key role in heart function can cause potentially life-threatening arrhythmia syndromes known as calmodulinopathy.
Calmodulinopathy is rare and causes arrhythmias that are poorly treated by current options. Boston Children’s cardiologist William Pu, MD, believes he has found a promising custom genetic treatment: antisense oligonucleotides that deplete the disease-causing gene product. Antisense oligonucleotides (ASO) are an emerging pharmaceutical option that target a disease at the RNA level, and Pu’s research points to its potential for improving the care of arrhythmias.
Three different genes (CALM1, CALM2, and CALM3) produce the identical protein, calmodulin (CaM). A damaging variant in one of these three genes causes calmodulinopathy. As Pu’s research showed, in both human cell and mouse disease models caused by a damaging variant in CALM1, an ASO effectively depleted the CALM1 gene product, and without affecting CALM2 or CALM3. This corrected arrhythmias caused by the CALM1 variant, yet was safe because CALM2 and CALM3 continued to produce normal levels of calmodulin protein.
“The study shows the strategy works,” Pu says. “Depleting both the wild type and the variant copies of the diseased gene is safe and effective for this disease because of the genetic redundancy provided by the other two unaffected genes.”
Targeting one gene to knock out many arrythmia variants
Pu, associate chair of cardiology for Basic and Translational Cardiovascular Research at Boston Children’s, and other researchers have been discovering the genetic causes of congenital heart disease (CHD). About 45% of CHD cases have an identifiable cause, including genetic variants affecting protein-coding genes.
Pu got interested in CaM intercellular protein as part of his work for Boston Children’s Center for Cardiovascular Genetics, which conducts genetic testing of families and helps coordinate the care of patients at the Benderson Family Heart Center.
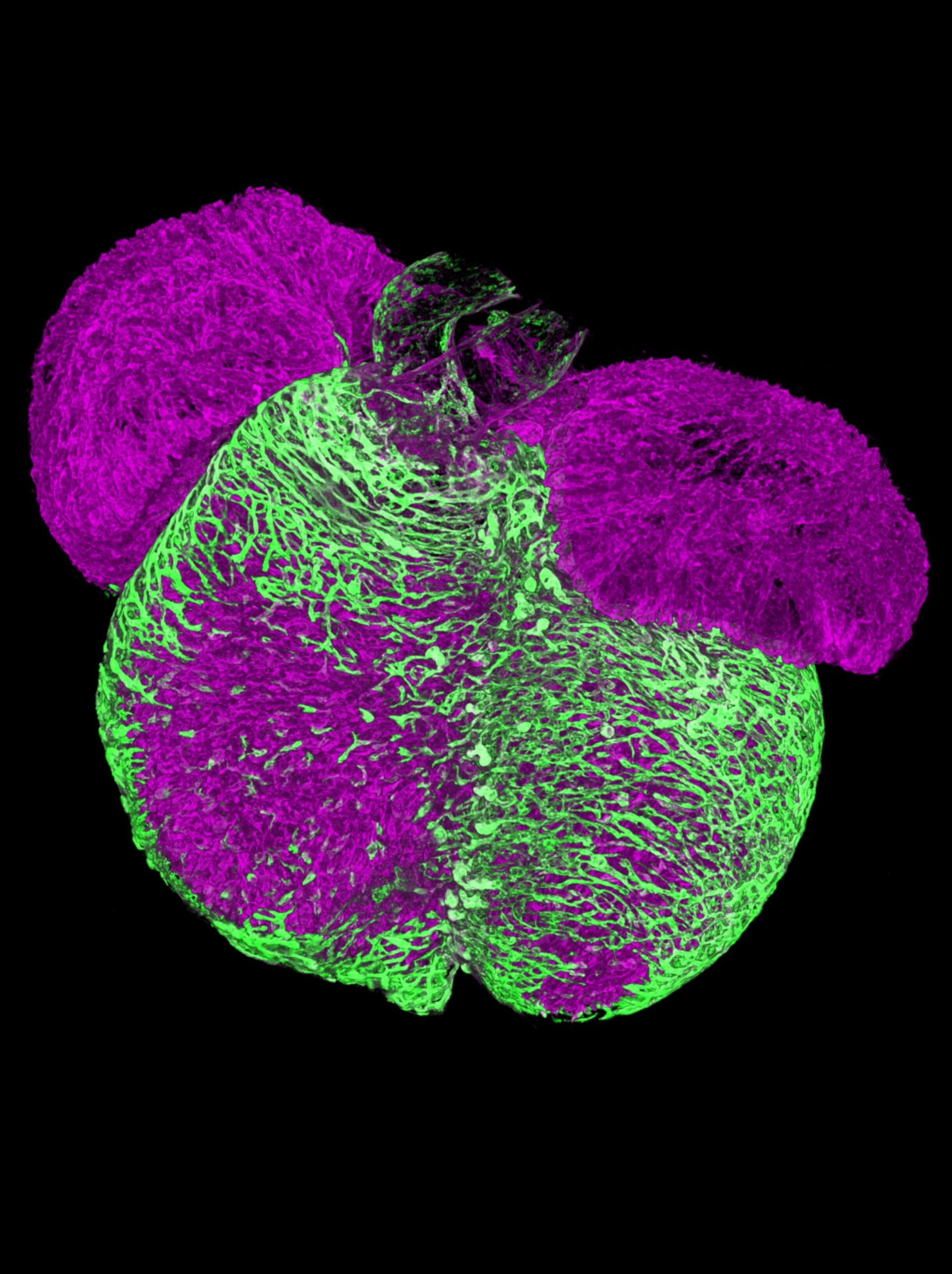
Cardiac cells release calcium to start a heart contraction. As part of that process, calmodulin binds calcium ions to mediate their signaling. Pu was struck by how the three separate genes—CALM1, CALM2, and CALM3—encode the same calmodulin protein. Variants in any one of those genes affect the binding and signaling processes, causing calmodulinopathy. The calmodulinopathy presents as inherited arrhythmias such as long QT syndrome and catecholaminergic polymorphic ventricular tachycardia (CPVT).
“As I learned about the disease, and the redundancy of three genes encoding the same protein, it made me think it was perfect for antisense oligonucleotide,” Pu recalls. That redundancy mattered, he says, because ASO doesn’t effectively distinguish single nucleotide differences.
Furthermore, targeting all variants in the affected CALM gene would allow the same ASO to be used for many patients, whereas an ASO designed for each different genetic variant would not. Because there are three CALM genes, it is possible to deplete the RNA made by one gene since the other two genes are able to continue to produce calmodulin.
Challenges still exist, but ASO has potential for heart treatment
Pu, his lab, and collaborating researchers from Boston Children’s Department of Cardiology and several other institutions believe they have created an ideal strategy for ASO to help treat calmodulinopathy. As the researchers detail in a study recently published in Circulation, they developed and tested ASOs in human-induced pluripotent stem cell–derived cardiomyocytes and mouse models of CALM1 pathogenic variants.
They found that ASO depletion of CALM1 is a potentially safe and effective way to erase the wild-type and mutated alleles, treating the disease without any detected toxicity. Removing CALM1 also did not affect the protein levels and functionality of CALM2 and CALM3. Testing the knockout in the mouse models was particularly powerful: It eliminated more than 90% of CALM1 and showed no signs of toxicity.
Current therapies for calmodulinopathy, such as beta-blockers and implantable cardiac defibrillators, are inadequate, Pu says. Patients using those therapies continue to experience arrhythmias. He hopes the new research successfully builds upon a growing movement that is exploring ASOs as a potential customized therapy for rare diseases.
Pu would next like to determine whether the genetic redundancy of the CaM protein could produce the same therapies for the pathogenic variants in CALM2 and CALM3. Beyond that, a next step for the larger research community is improving the delivery of oligonucleotide therapies to humans. Effective delivery of ASOs to muscle in patients remains a challenge, Pu says.
Although ASOs targeting liver cells are in clinical use and highly effective, so far the only oligonucleotide therapies targeting muscles are for Duchenne muscular dystrophy, and these have limited efficacy due to poor muscle uptake. Pu’s lab is working with other groups to develop a delivery method that would overcome the challenge.
The redundancy of CALM makes this ASO strategy for calmodulinopathy unique. The genes of many other heart conditions probably won’t allow for the depletion of wild-type and mutated alleles, Pu says. “But that doesn’t mean oligonucleotide therapies won’t be useful for other heart conditions. Being able to modulate the expression of some genes up or down by a small percentage or change the splicing of genes, as with Duchenne—those could be very powerful for the heart and muscle diseases.”
More information:
Raul H. Bortolin et al, Antisense Oligonucleotide Therapy for Calmodulinopathy, Circulation (2024). DOI: 10.1161/CIRCULATIONAHA.123.068111
Citation:
Research explores genetic treatment for rare arrhythmias (2024, October 2)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-explores-genetic-treatment-rare-arrhythmias.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.