A novel aqueous lubricant technology designed to help people who suffer from a dry mouth is between four and five times more effective than existing commercially available products, according to laboratory tests.
Developed by scientists at the University of Leeds, the saliva substitute is described as comparable to natural saliva in the way it hydrates the mouth and acts as a lubricant when food is chewed.
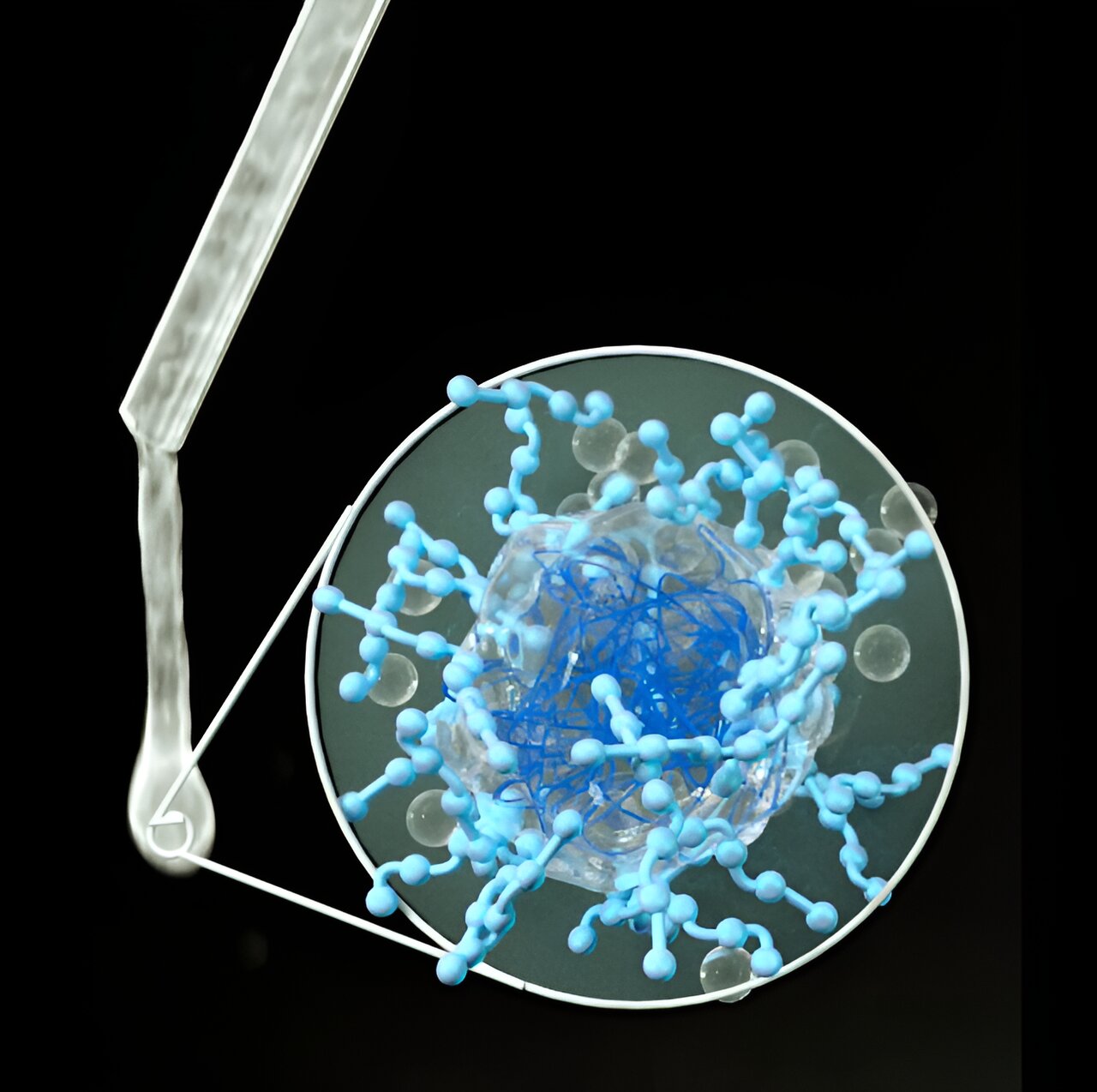
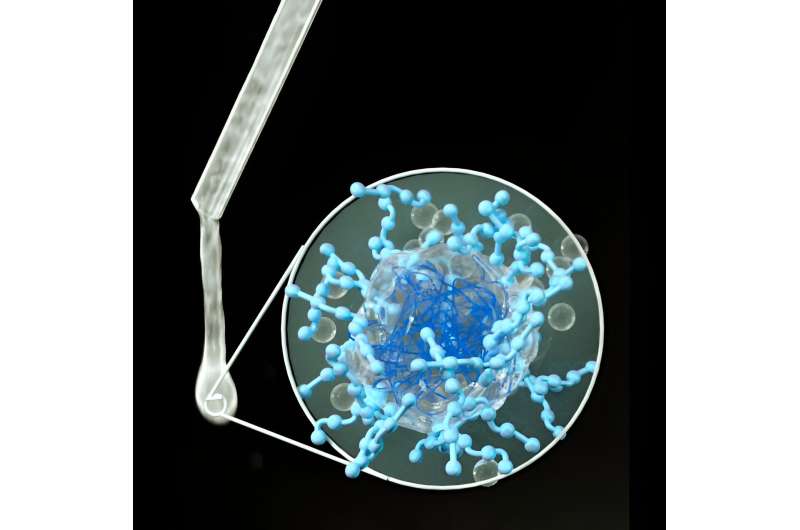
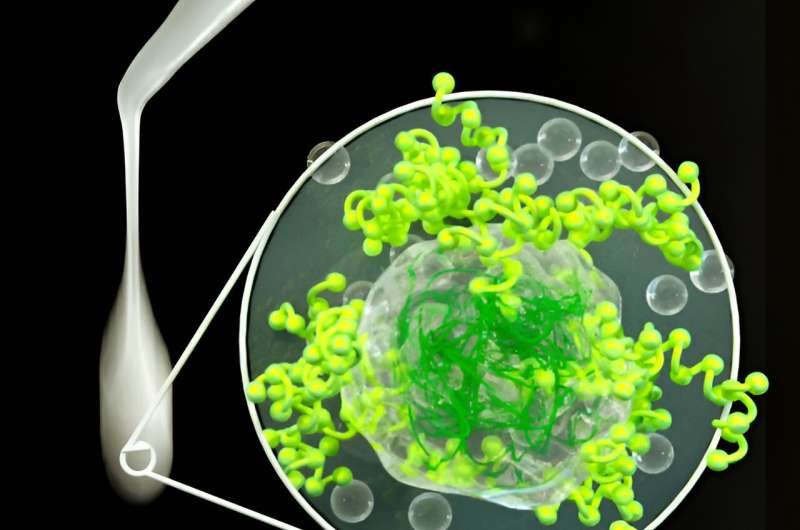
Under a powerful microscope, the molecules in the substance—known as a microgel—appear as a lattice-like network or sponge which bind onto the surface of the mouth. Surrounding the microgel is a polysaccharide-based hydrogel which traps water. This dual function will keep the mouth feeling hydrated for longer.
Professor Anwesha Sarkar, who has led the development of the saliva substitute, said, “Our laboratory benchmarking reveals that this substance will have a longer-lasting effect.
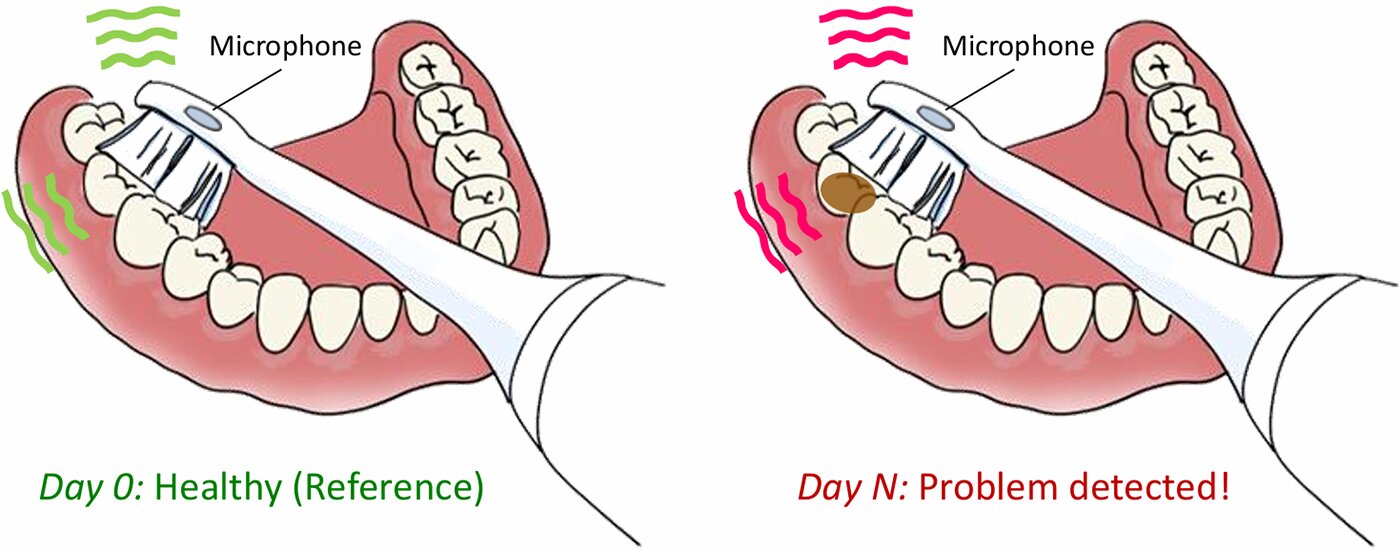
“The problem with many of the existing commercial products is they are only effective for short periods because they do not bind to the surface of the mouth, with people having to frequently reapply the substance, sometimes while they are talking or as they eat.
“That affects people’s quality of life.”
Results from the laboratory evaluation, “Benchmarking of a microgel-reinforced hydrogel-based aqueous lubricant against commercial saliva substitutes,” are reported in the journal Scientific Reports.
The performance of the newly developed substance in comparison to existing products is due to a process called adsorption. Adsorption is the ability of a molecule to bind to something, in this case the surface of the inside of the mouth.
Benchmark results
The novel microgel comes in two forms: one made with a dairy protein and the other a vegan version using a potato protein.
The new substance was benchmarked against eight commercially available saliva substitutes including Boots own brand product—Biotene; Oralieve; Saliveze; and Glandosane. All the benchmarking was done in a laboratory on an artificial tongue-like surface and did not involve human subjects.
The testing revealed the Leeds product had a lower level of desorption—the opposite of adsorption—which is how much lubricant was lost from the surface of the synthetic tongue.
With the commercially available products, between 23 to 58% of the lubricant was lost. With the saliva substitute developed at Leeds, the figure was just 7%. The dairy version slightly outperformed the vegan version.
Dr. Olivia Pabois, a Research Fellow at Leeds and first author in the paper, said, “The test results provide a robust proof of concept that that our material is likely to be more effective under real-world conditions and could offer relief up to five times longer than the existing products.
“The results of the benchmarking show favorable results in three key area. Our microgel provides high moisturization, it binds strongly with the surfaces of the mouth and is an effective lubricant, making it more comfortable for people to eat and talk.”
The substances used in the production of the saliva substitute—diary and plant proteins and carbohydrates—are non-toxic to humans and non-caloric.
Although testing of the new product has involved just laboratory analysis, the scientific team believe the results will be replicated in human trials.
The authors of the study are looking to translate the lubricant technology into commercially available products, to improve the quality of life of people who experience debilitating dry mouth conditions.
Xerostomia: Health care burden
A dry mouth or xerostomia, to give it its medical name, is a common condition which affects around one in ten of the population, and is prevalent among older people and people who have had cancer treatment or need to take a mix of medicines.
In severe cases, a dry mouth results in people having discomfort swallowing and leads to malnutrition and dental problems, all of which increase the burden on health care systems.
More information:
Olivia Pabois et al, Benchmarking of a microgel-reinforced hydrogel-based aqueous lubricant against commercial saliva substitutes, Scientific Reports (2023). DOI: 10.1038/s41598-023-46108-w
Citation:
Proof of concept of new material for long lasting relief from dry mouth conditions (2023, November 20)
retrieved 5 October 2024
from https://medicalxpress.com/news/2023-11-proof-concept-material-relief-dry.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.