For years, many people with Alzheimer’s disease have been diagnosed clinically and confirmed at autopsy. Now Alzheimer’s disease pathology can be identified with relatively high accuracy via a blood test that has the potential for widespread use in practice.
However, while Alzheimer’s biomarkers can measure the presence of amyloid and tau in the brain, salient issues including appropriate use for patients with other diseases that may alter pathology, prediction accuracy and how best to employ information obtained from biomarker testing have not yet been resolved.
In an article highlighting the issues related to use of this new diagnostic tool, applied aging researcher Nicole R. Fowler, Ph.D., of the Regenstrief Institute and Indiana University School of Medicine, and Michelle Mielke, Ph.D., chair of the department of epidemiology and prevention at Wake Forest University School of Medicine, outline factors to be considered in preparation for widespread implementation of Alzheimer’s biomarker testing in real-world, clinical populations.
“Alzheimer disease blood biomarkers: considerations for population-level use” is published in Nature Reviews Neurology.
They note that biomarkers present an unprecedented opportunity to improve the timeliness and accuracy of Alzheimer’s diagnosis at the population level, including in low-resource settings, but urge reflection on a range of factors before widespread adoption.
“Blood for biomarker testing can be drawn just like any other lab and examined for presence of amyloid or tau in the brain, the main pathologies for Alzheimer’s disease,” said Dr. Fowler. “But while it’s a much less invasive and a much more scalable test than collecting cerebral spinal fluid, we need to create appropriate use guidelines for blood-based biomarkers to aid in the diagnosis of Alzheimer’s disease.
“We’ve begun that process by outlining some of the areas we need to look into as we begin to take advantage of this new tool. Biomarkers may be a very appropriate test early in the cognitive change process to determine what is causing cognitive concerns, to help patients on a path of slowing the disease and being evaluated for treatment.”
“Much of the research to date on Alzheimer’s disease blood-based biomarkers have been conducted on relatively healthy, higher educated and well characterized participants at specialty memory clinics,” stated Dr. Mielke.
“Much work is needed to understand how to best implement these blood biomarkers among older adults with multiple chronic conditions and cognitive impairment, including among underrepresented minority groups. There are ethical issues to consider as well as some chronic conditions that could affect the interpretation of the biomarker and lead to false positive or false negative diagnoses.”
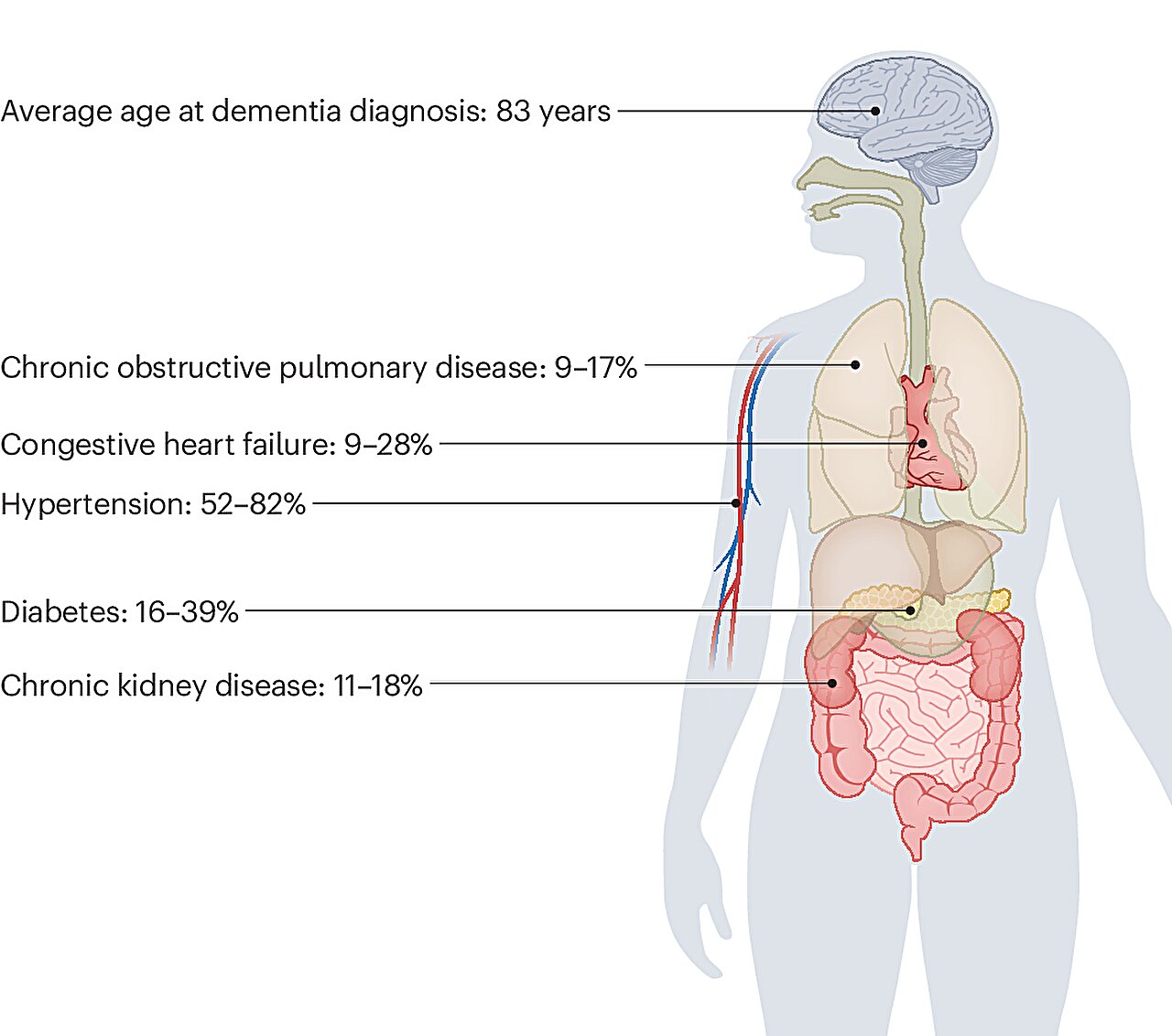
In their review article, Drs. Fowler and Mielke discuss the importance of considering numerous confounding factors to consider with the interpretation of biomarker tests including patient sex and race or ethnicity and the simultaneous presence of chronic medical conditions that are common in older adults.
They report that the characteristics of typical primary care patients with cognitive impairment often differ from the patient populations that have been used in Alzheimer’s biomarker research studies and emphasize the need for population health studies to be more reflective of individuals seeking diagnoses to understand how best to implement this new technology in the primary care setting.
Stressing the importance of mitigating the potential for false-positive or false-negative results due to imperfect testing accuracy, they conclude by discussing broader issues such as ethics, patient and provider preference, incidental findings and dealing with indeterminate results.
Key points noted by Drs. Fowler and Mielke:
- Numerous studies have demonstrated the clinical utility and accuracy of blood biomarkers for the detection of Alzheimer pathology among patients with signs of cognitive impairment.
- Most research studies to date have focused on specialty clinic—such as neurology—populations and are not generalizable to typical primary care patients with cognitive impairment symptoms so an urgent need exists to test these biomarkers with this population.
- Chronic kidney disease, obesity and cardiovascular conditions or some medications can elevate or lower Alzheimer blood biomarker levels and need to be taken into consideration to avoid false-positive or false-negative diagnoses. Understanding how to interpret these levels in the context of multiple chronic conditions is crucial for diagnosing Alzheimer’s among older adults.
- Other factors that might influence Alzheimer’s disease levels include gender and race or ethnicity, although findings on these associations have been inconsistent.
- A positive blood biomarker test might indicate the presence of Alzheimer pathology but could be an incidental finding so the test must be considered in the context of all other symptoms.
- Policies must be developed to protect patients who have positive results added to their medical records so that they do not lose access to insurance, disability or other rights.
More information:
Michelle M. Mielke et al, Alzheimer disease blood biomarkers: considerations for population-level use, Nature Reviews Neurology (2024). DOI: 10.1038/s41582-024-00989-1
Citation:
Preparing for widespread use of biomarkers to diagnose Alzheimer’s disease (2024, September 18)
retrieved 7 October 2024
from https://medicalxpress.com/news/2024-09-widespread-biomarkers-alzheimer-disease.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.