Tackling brain cancer is complicated, but groundbreaking new research could help add another tool to the cancer-fighting arsenal.
A team from Georgia Tech and Virginia Tech published a paper in APL Bioengineering in May that explores a new option that could one day be used to target glioblastoma, a deadly and fast-growing brain tumor.
Supported by National Institutes of Health grants, this work stems from past research on high frequency irreversible electroporation, better known as H-FIRE. H-FIRE is a minimally invasive process that uses non-thermal electrical pulses to break down cancer cells.
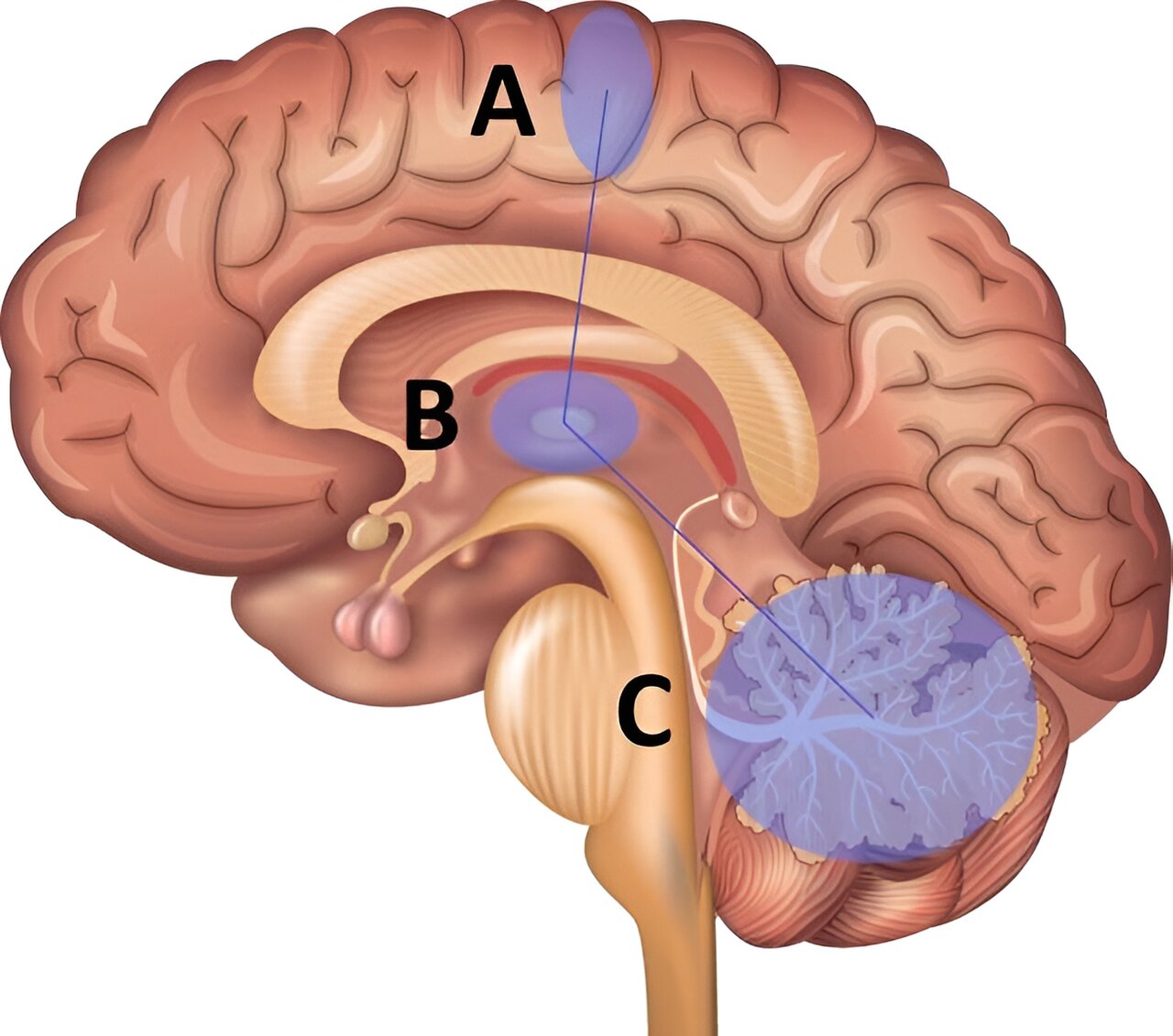
Treating any type of cancer isn’t easy, but when it comes to brain cancers, the blood-brain barrier adds an extra challenge. The barrier defends the brain against toxic material — but that’s not always a positive thing.
“Mother Nature designed it to prevent us from poisoning ourselves, but unfortunately, the way that works, it also excludes about 99 percent of all small-molecule drugs from entering the brain and achieving adequate concentrations to elucidate their therapeutic effect. That’s particularly true for chemotherapeutics, biologics, or immunotherapies,” said John Rossmeisl, the Dr. and Mrs. Dorsey Taylor Mahin Professor of Neurology and Neurosurgery at the Virginia-Maryland College of Veterinary Medicine. Rossmeisl is one of the paper’s coauthors.
The square-shaped wave typically used with H-FIRE performs double dut: It disrupts the blood-brain barrier around the tumor site while destroying cancer cells. However, this was the first study to use a sinusoidal wave to disrupt the barrier. This new modality is called burst sine wave electroporation (B-SWE).
The researchers used a rodent model to study the effects of the sinusoidal wave versus the more conventional, square-shaped wave. They found that B-SWE resulted in less damage to cells and tissue but more disruption of the blood-brain barrier.
In some clinical cases, both ablation and blood-brain barrier disruption would be ideal, but in others, blood-brain barrier disruption may be more important than destroying cells. For example, if a neurosurgeon removed the visible tumor mass, the sinusoidal waveform could potentially be used to disrupt the blood-brain barrier around the site, allowing drugs to enter the brain and eliminate the last of the cancer cells. B-SWE could result in minimal damage to the healthy brain tissue.
Research indicates that the conventional square waveforms show good blood-brain barrier disruption, but this study finds even better blood-brain barrier disruption with B-SWE. This could allow more cancer-fighting drugs to access the brain.
“We thought we had that problem solved, but this shows you that with some forward thinking, there’s always potentially better solutions,” said Rossmeisl, who also serves as associate head of the Department of Small Animal Clinical Sciences.
During the study, the researchers hit a snag: In addition to more blood-brain barrier disruption, they found that the sinusoidal wave also caused more neuromuscular contractions. These muscle contractions run the risk of damaging the organ. However, by tweaking the dose of B-SWE, they were able to reduce the contractions while providing a level of blood-brain barrier disruption similar to that of a higher dose.
The next step in this research is to study the effects of B-SWE using an animal model of brain cancer to see how the sinusoidal waveform stands up against the conventional H-FIRE technique.
The project was spearheaded by first author Sabrina Campelo while she completed her Ph.D. at the Virginia Tech-Wake Forest University School of Biomedical Engineering and Sciences. Campelo is now a postdoctoral fellow at the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University.