A team led by Dr. Elena Cano in the Integrative Vascular Biology Lab of Professor Holger Gerhardt at the Max Delbrück Center in Berlin has elucidated the mechanism via which new arteries form in the heart. The finding, published in Circulation Research, fills in an important gap in our understanding of how coronary arteries develop and could help improve treatments that aim to heal damage to heart muscle caused by a heart attack or stroke—leading causes of death and disability worldwide.
A heart attack or stroke can cause tissue within heart muscle to die. As a result, the blood supply to the heart diminishes, leading to permanent disability. Although some tissue does spontaneously heal by growing new blood vessels, the extent is often inadequate to completely restore blood supply. Current therapies focus on managing symptoms and slowing heart disease.
Researchers have attempted various methods to coax new blood vessels to grow in damaged heart tissue. However, they have not been able to establish a stable, mature vascular network that improves the heart’s function, says Cano. One major drawback has been the lack of deeper understanding of the intricate molecular, cellular, and structural cues that vascular cells use to build a hierarchical blood vessel network.
Applying single-cell sequencing to the problem
While studying how tissues vascularize, Cano discovered a type of pre-arterial cell in her samples that appeared to play a major role in growing new arteries. These pre-arterial cells had already been reported by other researchers. But Cano wanted to study them with new technology.
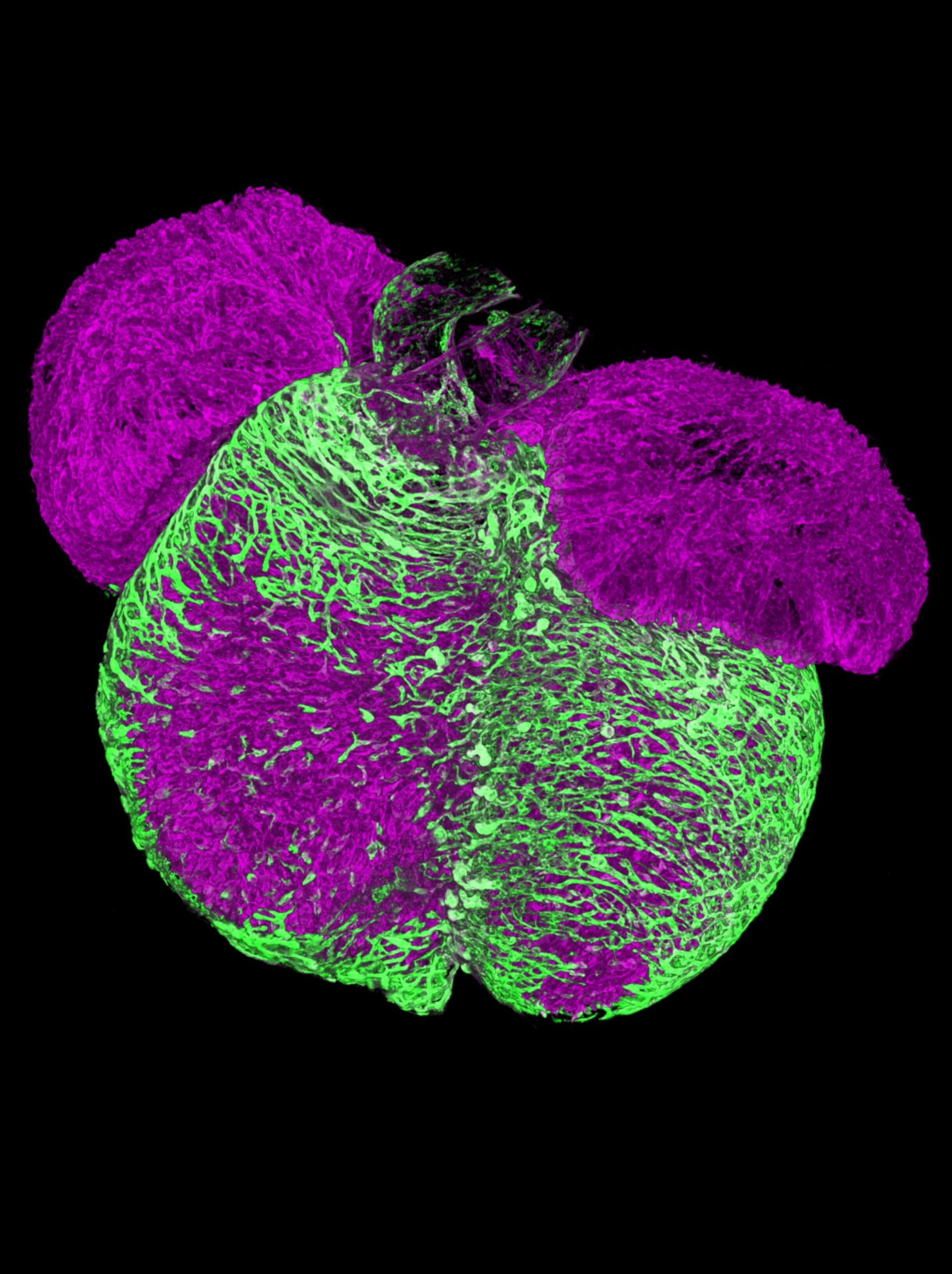
Using single-cell sequencing to analyze the transcriptome of cardiac cells taken from mice at different stages of development, the team of researchers showed that these cardiac pre-arterial cells develop from “tip cells”—specialized cells that sense environmental cues to drive growing vessels into specific directions. The team also used 3D spatiotemporal mapping to confirm their results. Moreover, they showed that these pre-arterial cells were already “marked” to develop into arterial cells, which belies current thinking about how arteries develop.
It had been thought that new arteries form their unique characteristics, such as length and diameter, based purely on mechanical cues, such as the velocity of the fluid flowing through them. However, “this study shows that pre-arterial cells already have characteristics of arteries before any fluid flows through them,” Cano says.
The researchers also reanalyzed previously published single-cell data collected by researchers in the U.K. from human embryonic heart tissue. They then compared it to their own data collected from mouse heart tissue damaged by heart attack. They found that new arteries formed in the human embryonic tissue via the same mechanism as after damage from a heart attack in mice.
“We show that not only is this mechanism conserved between mice and humans during development, but it also persists throughout life and becomes activated after a heart attack,” says Cano.
Implications for treatment
Understanding how coronary arteries naturally form and regenerate opens the possibility of developing treatments that stimulate these regenerative pathways, potentially reversing heart muscle damage, says Cano.
“Now we know that it is not only flow that signals vascular endothelial cells to become arteries, but that tip cells transition into pre-arterial cells to eventually become arteries,” says Gerhardt. “Surprisingly, we find that not all tip cells have the capacity to form arteries, raising the prospect of selectively increasing this pool of cells for therapeutic purposes.”
“This is a step forward,” Cano adds. “It is a new mechanism that we can potentially tweak during regeneration to see whether we can form new arteries for optimal restoration of blood supply.”
More information:
Elena Cano et al, Intramyocardial Sprouting Tip Cells Specify Coronary Arterialization, Circulation Research (2024). DOI: 10.1161/CIRCRESAHA.124.324868
Citation:
New clues on how the heart makes arteries (2024, August 30)
retrieved 1 September 2024
from https://medicalxpress.com/news/2024-08-clues-heart-arteries.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.