A major challenge for cancer surgeons is to determine exactly where a tumor starts and where it ends. Removing too much tissue can impair normal functions, but not taking enough can mean the disease could recur. The “MasSpec Pen,” a handheld device in development, could someday enable surgeons to distinguish between cancerous and healthy tissue with greater certainty in seconds, while in the operating room. Today, researchers report first results of its use in human surgeries.
The researchers will present their findings at the American Chemical Society (ACS) Fall 2019 National Meeting & Exposition.
“It’s been shown with extensive clinical data that highly effective surgeries are those that remove the most cancer, but also preserve the most normal tissue,” says principal investigator Livia Eberlin, Ph.D. “We created the MasSpec Pen because we thought it would be incredible if there was a technology that could actually provide molecular information right in the operating room in living tissues within a time frame that could expedite surgical decisions.”
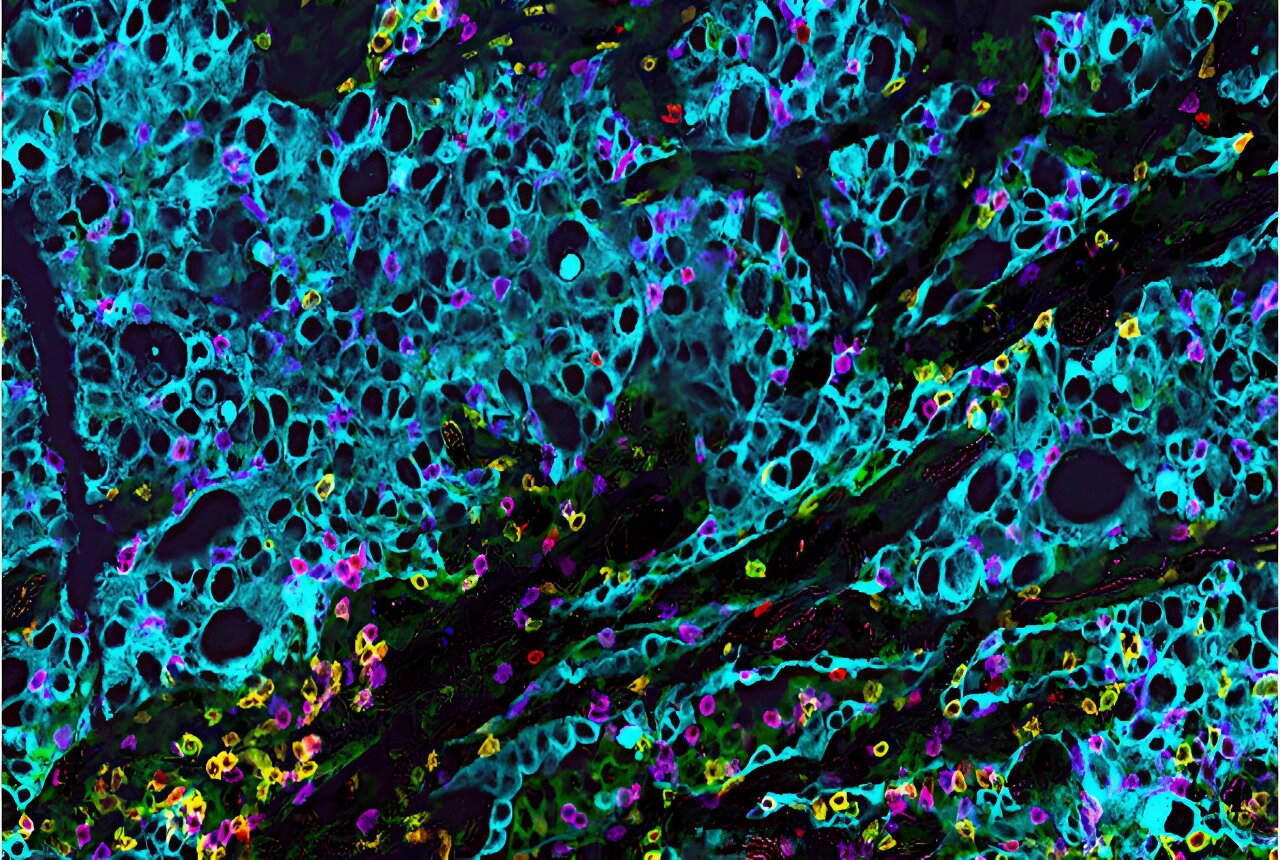
Surprisingly, the most common method that medical professionals currently use to determine tumor margins or verify a diagnosis is 100 years old: histopathology. With this technique, a tissue sample is extracted during surgery and taken to a laboratory. The sample is flash-frozen, sectioned, stained and examined with a microscope. In total, this procedure can take an average of 30 minutes. Meanwhile, the patient, who is still under anesthesia, and the surgeon are left waiting. In addition, while histopathology is effective for many surgeries, especially for cancers, the process can be subjective because artifacts from the freezing process can complicate interpretation, Eberlin explains.
To overcome these challenges, Eberlin and colleagues at the University of Texas at Austin developed the MasSpec Pen, a handheld and biocompatible device connected to a high-performance mass spectrometer. The device rapidly identifies the molecular profile of tissue exposed during a surgery by first depositing a small droplet of water on the tissue surface for about three seconds. Next, the droplet is transferred to the mass spectrometer, where molecules from the tissue are identified. Finally, machine learning algorithms comb through the molecular information and provide a predictive diagnosis that surgeons can act on.
“We have developed the MasSpec Pen so that the surgeon just has to touch the tissue with the pen, and trigger the system with a foot pedal,” Eberlin says. “From there, everything is coded and automated so that the whole process is completed in under 10 seconds.”
So far the MasSpec Pen has been tested on more than 800 human tissues ex vivo, including normal and cancerous breast, brain, pancreatic, thyroid, lung and ovarian tissues. The team is now testing the MasSpec Pen in vivo, in an ongoing clinical study at the Texas Medical Center with human patients during thyroid, breast and pancreatic cancer surgeries. Freshly excised patient tissue also is being analyzed and is showing promising results.
“We are continuing research and development of this technology in my lab by continuing to improve our technology and validating its performance across different cancer types,” Eberlin says. “We are also exploring new applications in surgery including minimally invasive surgical procedures, as well as outside the operating room in forensics and agricultural applications.”