A survey of 607 women who suffer from severe migraine found twenty percent of the respondents are currently avoiding pregnancy because of their migraines. The women avoiding pregnancy due to severe migraine tend to be in their thirties, are more likely to have migraine triggered by menstruation, and are more likely to have very frequent attacks (chronic migraine) compared to their counterparts who are not avoiding pregnancy, according to a new study in Mayo Clinic Proceedings. Their decision appears to be based on perceived fears about their own health and the health of their child, even though evidence shows that migraine improves in up to 75 percent of women during pregnancy.
Migraine is one of the leading causes of disability worldwide, particularly affecting women during their childbearing years. “A large number of women with migraine might avoid pregnancy due to migraine. So they can make informed decisions, it is important that women with migraine have access to reliable information about the relationship between migraine and pregnancy,” explained lead author Ryotaro Ishii, MD, PhD., a visiting scientist at Mayo Clinic, Phoenix, AZ, USA.
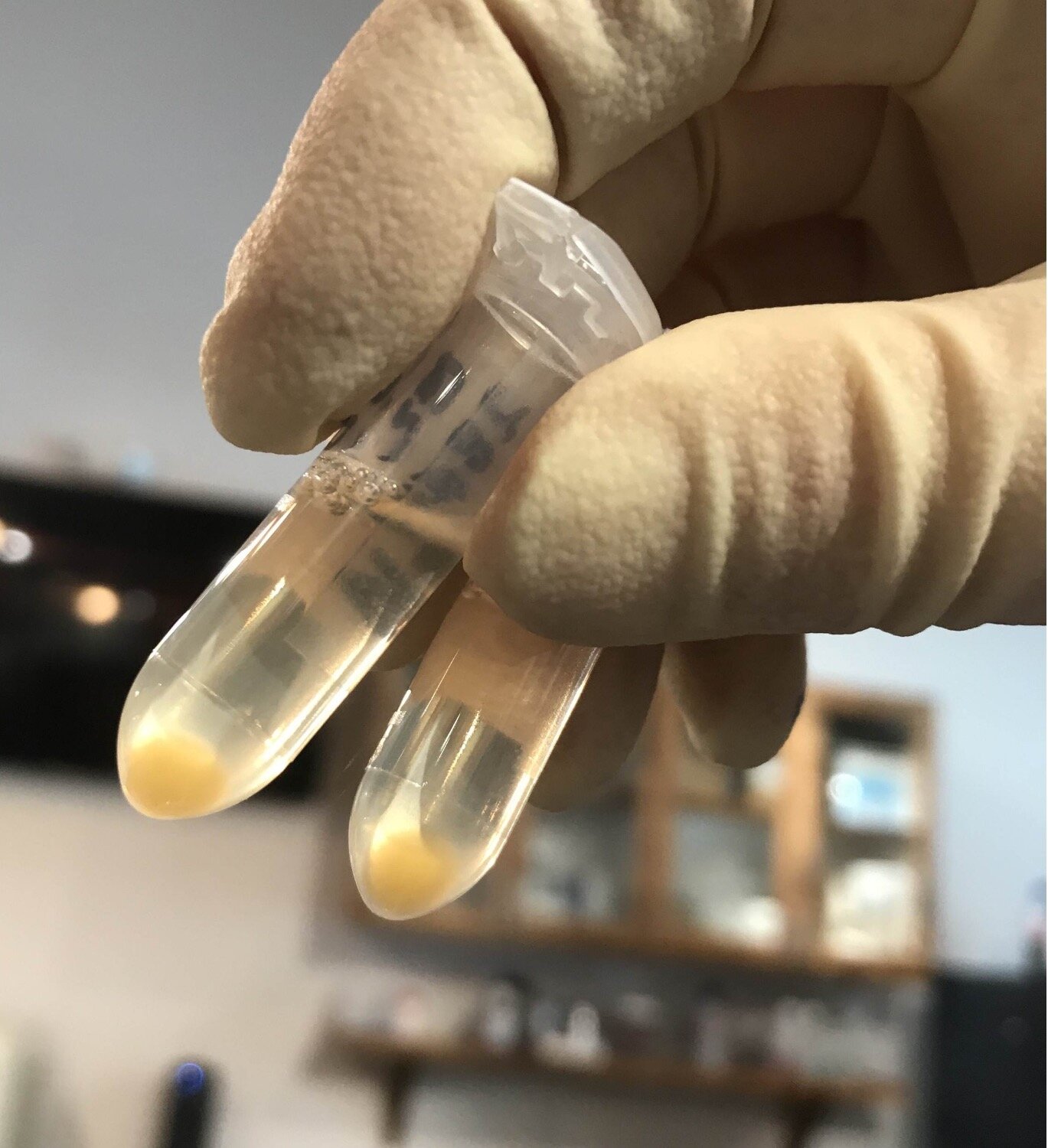
The study investigated the impact of migraine on pregnancy plans among patients being treated in headache specialty clinics and enrolled in the American Registry for Migraine Research (ARMR), the American Migraine Foundation’s national prospective longitudinal patient registry and biorepository. Corresponding author Todd J. Schwedt, Mayo Clinic, Phoenix, AZ, USA, and Principal Investigator of ARMR, remarked, “ARMR is a multicenter patient registry that collects in-depth clinical data, biospecimens, and neuroimaging data from a large number of individuals with migraine and other headache types. ARMR provides deep insights into the clinical manifestations, management, and outcomes of patients with headache.”
Patients provide demographic data when they enroll in ARMR and complete questionnaires about their medical history. A family planning questionnaire is included. The database includes a specialist’s diagnosis of migraine subtypes, such as migraine with aura, migraine without aura, chronic migraine (at least 15 headache days per month), and/or menstrual migraine.
The family planning questionnaire was completed by 607 patients within ARMR between February 2016 and September 2019. Patients were asked, “Have migraines impacted your plans for pregnancy?” They selected one of the following answers: “Avoid pregnancy — Significant;” “Avoid pregnancy — Somewhat;” “No Impact/Not Sure;” “Increased Desire to Get Pregnant — Somewhat;” and “Increased Desire to Get Pregnant — Significant.” Six individual questions that asked about how migraine might impact pregnancy, the ability to raise a child, and the child’s health were rated on a scale from “Strongly agree” to “Strongly disagree.”
Patients were divided into two groups according to whether or not they reported avoiding pregnancy because of migraine. Twenty percent of the patients indicated that they avoided pregnancy because of their migraine. The average age for those who reported avoiding pregnancy was 37.5 years, younger than that of the group who reported no impact of migraine on their pregnancy plans (47.2 years). Women who experienced migraine attacks associated with their menstrual cycle more commonly avoided pregnancy compared to those who did not experience menstrual-related migraine attacks. They more frequently reported a history of depression, a higher monthly frequency of days with headache, and higher migraine-related disability over the three previous months.
Among those who avoided pregnancy due to migraine, 72.5 percent believed that their migraine would be worse during or just after pregnancy, 68.3 percent believed their disability would make pregnancy difficult, and 82.6 percent believed that the disability caused by migraine would make raising a child difficult. There were also concerns that medications they take would negatively affect their child’s development and that they would pass on genes to their baby that increase the risk of the child having migraine.
The investigators noted that research does not support what the patients in the ARMR believed about the impact of migraine on pregnancy. About one half to three fourths of women with migraine experience a marked improvement during pregnancy, with a significant reduction in the frequency and intensity of attacks according to published literature. Because the prognosis of migraine during pregnancy is generally good, it may be possible to limit the use of medications, thereby reducing the risk of medication-related adverse events. Migraine does not appear to increase the risk for fetal malformations, although some studies suggest a small increase in poor pregnancy and fetal outcomes.
The authors cautioned that because ARMR patients are enrolled from specialty headache centers and are more severely affected by migraine, the results cannot necessarily be generalized to the general population of people with migraine. There may be certain patient characteristics associated with an individual being more likely to enroll.
It is essential that women of childbearing potential with migraine receive education about the potential impact of migraine on pregnancy, the authors observed. “As the leading cause of years lived with disability in the world, and one that affects one in three women during their lifetime, these data highlight the substantial impact migraine has on pregnancy and family planning,” added co-author David Dodick, MD, Mayo Clinic, Phoenix, AZ, USA, and Principal Investigator of ARMR. “Clinicians must be alert to and proactively manage these important concerns of their female patients.”
“This study is a testament to the unrelenting, destructive nature of this chronic invisible diagnosis, which can permeate all aspects of life if left unchecked, including potentially depriving women of the opportunity of motherhood should they desire as well as other important relationships,” commented Rashmi B. Halker Singh, MD, Department of Neurology, Mayo Clinic, Phoenix, AZ, USA, and Joseph I. Sirven, MD, Department of Neurology, Mayo Clinic, Jacksonville, FL, USA, in an accompanying editorial. “We need to not only support women who have migraine by addressing this patient education gap and improving our treatments to better meet their needs, but also must be deliberate in our efforts to improve societal understanding and acceptance of this prevalent neurobiological disease.”