Pete Williams is one of few researchers in Sweden concentrating on glaucoma. The goal is an effective treatment, something that stops the degenerative process in the nerve cells of the eye.
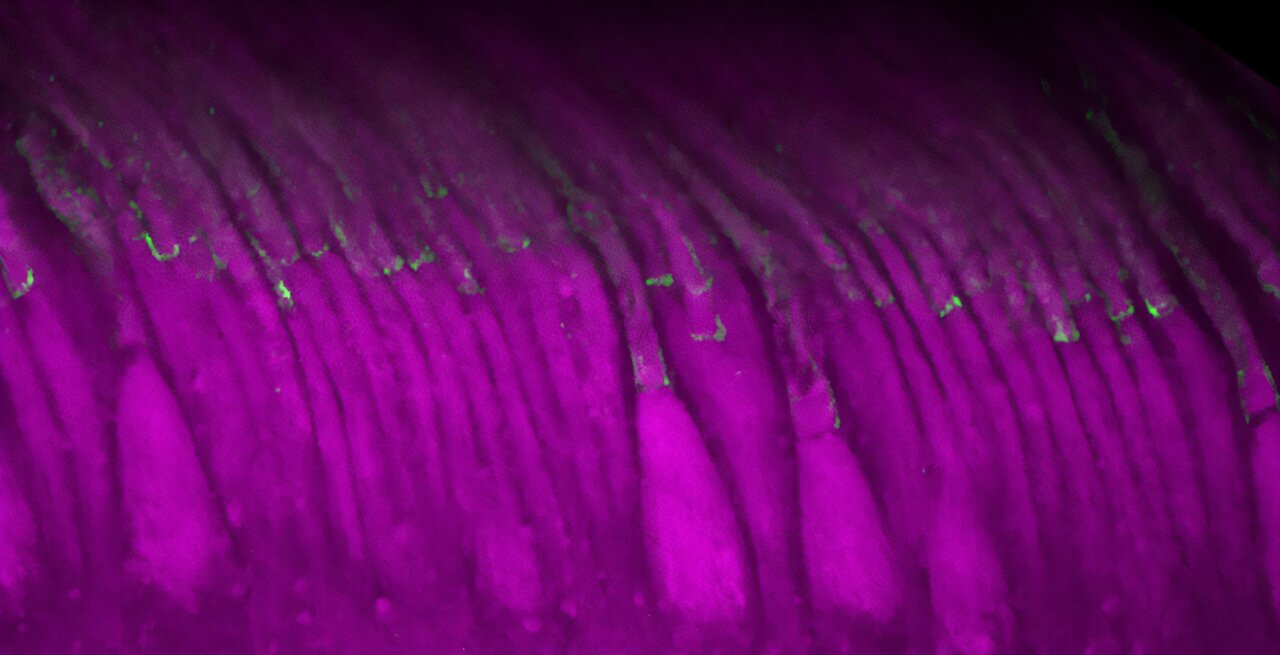
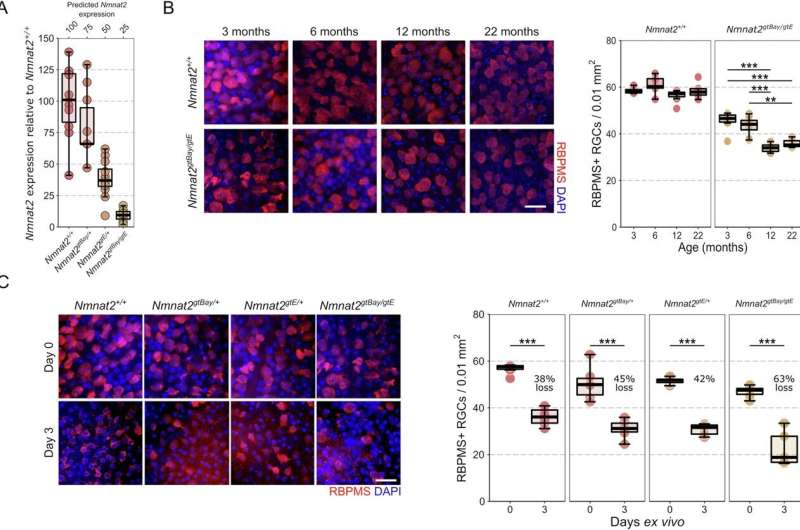
Williams is the senior author of a new paper in Nature Communications on how deficiency of the enzyme NMNAT2 renders the nerve cells of the eye vulnerable to neurodegeneration and could be a key in the search for a treatment.
Glaucoma is very common. Eighty million people worldwide have the eye disease (an estimated 100–200,000 in Sweden alone). There is no cure, but there are treatments that lower the pressure in the eye and that can slow down the progression of the disease, which otherwise leads to irreversible blindness.
Not always treatable
“Most people who have heard of glaucoma believe that it can be treated with eye drops and surgery. Unfortunately, this is not entirely true. For many of the patients, the treatment lowers eye pressure but doesn’t prevent further vision loss,” says Pete Williams.
Knowledge about glaucoma has taken time to develop because the disease progresses slowly. This means that in the past, it took many years before researchers could see if a particular treatment had any effect. However, in the last decade or so, the availability of instruments that measure changes in the eye much earlier than the patient experiences them has given new impetus to research into eye disease.
The importance of NAD
In the 1980s, research into neurodegenerative diseases discovered a link with NAD, a co-enzyme, i.e. a molecule that binds to an enzyme and makes it active. Williams’ group was the first to show that NAD levels were low in animal models of glaucoma.
“NAD has many important functions in the body. A lack of it is important for neuronal health and survival in many diseases, but we don’t yet know how to use this information to create a better treatment,” says Williams.
When the body makes NAD, it uses an enzyme NMNAT1. However, in neurons, it needs another enzyme: NMNAT2 (which is only found in neurons).
“In our recent paper in Nature Communications, we show that NMNAT2 is needed to protect neurons in the eye and that gene therapy can be used to increase levels,” says Williams.
The research team is now moving on to try to develop new substances that target NMNAT2 in nerve cells.
“We believe these compounds could be a starting point for future glaucoma treatment,” he adds.
More information:
James R. Tribble et al, NMNAT2 is a druggable target to drive neuronal NAD production, Nature Communications (2024). DOI: 10.1038/s41467-024-50354-5
Citation:
Gene therapy shows promise in glaucoma research (2024, August 7)
retrieved 21 September 2024
from https://medicalxpress.com/news/2024-08-gene-therapy-glaucoma.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.