As the Democratic Republic of Congo launches a vaccination campaign amid a flare-up of the sometimes deadly illness mpox, AFP looks at how the virus developed.
Several mpox epidemics have broken out, mainly in Africa, since it first emerged in humans in 1970.
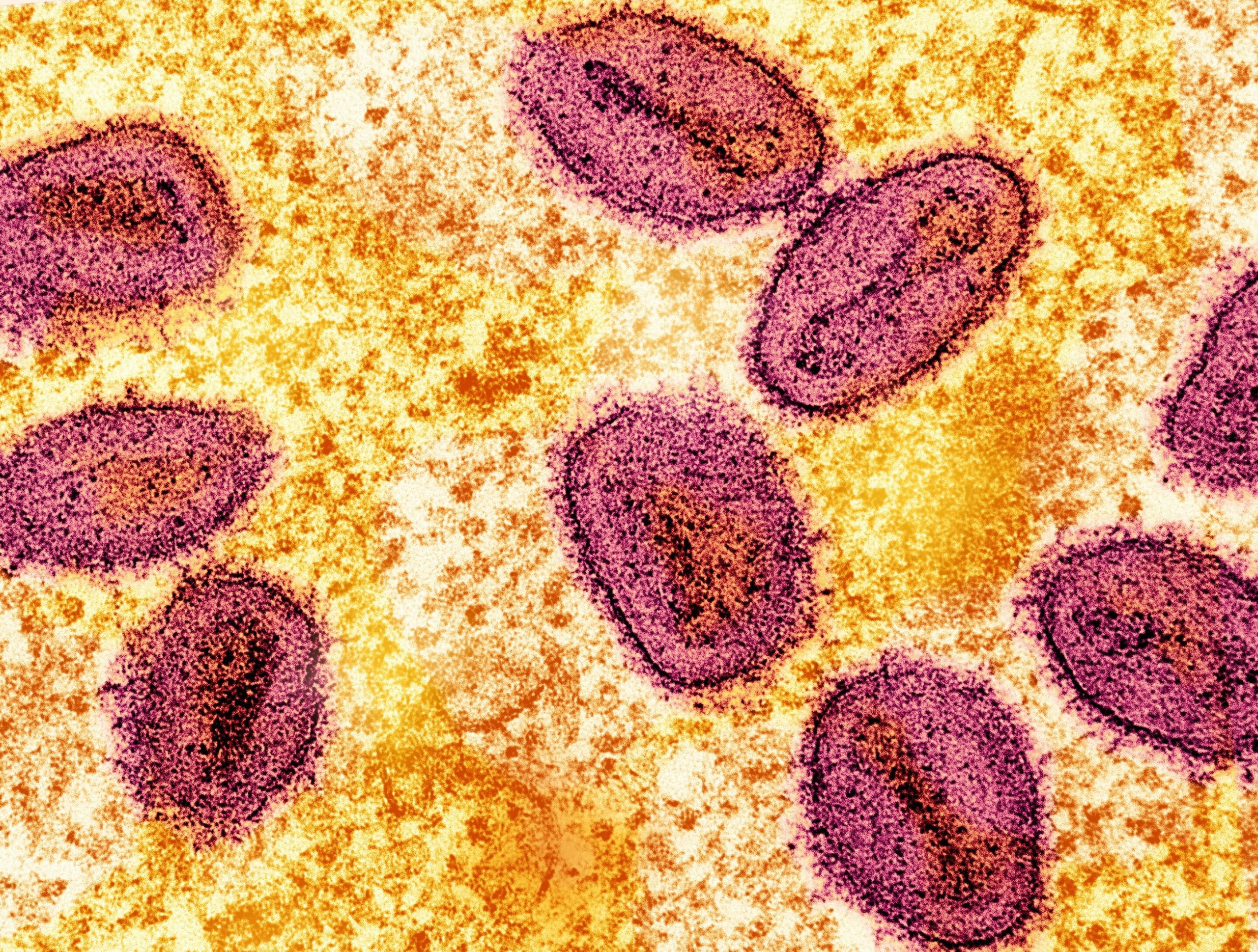
The disease, originally named Monkeypox, spreads through close physical contact with infected people or animals, causing fever, muscle pains and painful skin lesions.
First discovered in a monkey in 1958, it is related to, but far less severe than, the deadly smallpox virus, which was eradicated in 1980.
The World Health Organization said in November 2022 that it should be called “mpox”, which it considers less of a stigma.
1970: first case
The disease was first detected in humans in the DRC, then known as Zaire, in 1970, according to the WHO.
There are two virus subtypes—clade 1 and clade 2.
For decades, there have been sporadic cases of clade 1 in central Africa’s Congo Basin, and of clade 2 in parts of west Africa.
2003: first outbreak outside Africa
In June 2003, the disease surfaced for the first time outside Africa, in the United States.
It is believed to have spread after rodents, imported into the US from Ghana, infected prairie dogs.
The US Centers for Disease Control and Prevention (CDC) reported 87 cases, of which 20 were confirmed, but no fatalities.
2017: epidemic in Nigeria
2017 brought a major outbreak in Nigeria, with more than 200 confirmed cases, 500 suspected cases and a fatality rate of around three percent, the WHO said.
Over the next five years, sporadic cases were reported around the world in travelers arriving from Nigeria, notably in Britain, Israel, Singapore and the United States.
May 2022: surge outside Africa
From May 2022, clade 2 spread around the world, mostly affecting gay and bisexual men in Europe and the United States.
Clade 2 appears to spread mainly through close and prolonged contact, notably sexual intercourse. People with several partners are most at risk.
In July 2022, the WHO declared a Public Health Emergency of International Concern—its highest level of alarm.
Vaccination and awareness drives in many countries helped stem the number of worldwide cases and the WHO lifted that emergency in May 2023 after reporting 140 deaths out of roughly 87,400 cases.
2024: new global alert
In 2024 a new two-pronged epidemic broke out mainly in the DRC.
As well as clade 1, which mainly affects children, a new strain emerged in the DRC, called clade 1b. Clade 1b cases have also been recorded in nearby Burundi, Kenya, Rwanda and Uganda—none of which had previously detected mpox.
The WHO declared another international emergency in mid-August.
DRC is at the epicenter of the mpox outbreak and has recorded more than 30,000 cases, as well as 988 deaths, since January, according to its health minister.
According to the African Union’s health watchdog, Africa CDC, on October 3, some 34,297 cases, all strains, have been recorded in 16 countries across the continent since January.
A first vaccination campaign started on September 17 in Rwanda targeting people at high risk.
In the DRC a targeted vaccination campaign started on October 5. The country has received 265,000 doses of vaccines from the European Union and the United States. Washington plans to donate one million doses to African nations.
© 2024 AFP
Citation:
Mpox epidemic: from first cases to vaccinations (2024, October 6)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-mpox-epidemic-cases-vaccinations.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.