The BASHIR™ Endovascular Catheter (THROMBOLEX, Inc.), recently approved by the U.S. Food and Drug Administration (FDA), is paving the way to more effective and safe treatment for acute pulmonary embolism. Already shown to be effective for reducing blockages in lung arteries, new research at the Lewis Katz School of Medicine at Temple University shows that the BASHIR™ catheter also reduces blockages in the smaller segmental pulmonary artery branches. These branches are ultimately responsible for oxygenating the blood in the lungs.
The new study, which was part of the National Institutes of Health-sponsored multicenter RESCUE clinical trial, further showed a correlation between decreased numbers of blockages in the small lung arteries and functional recovery of the right ventricle of the heart, which pumps blood into the main pulmonary artery of the lungs. Compared to other devices, the BASHIR™ catheter also had significantly lower bleeding rates, a key advance in acute pulmonary embolism treatment. The findings are described in JACC: Advances.
“Blockages in these smaller, distal pulmonary arteries have never previously been explored in patients treated for acute pulmonary embolism,” explained Riyaz Bashir, MD, FACC, Professor of Medicine, Director of Vascular and Endovascular Medicine in the Section of Cardiology, Department of Medicine at the Lewis Katz School of Medicine and Temple University Hospital, co-inventor of the BASHIR™ Endovascular Catheter, and first author on the new report.
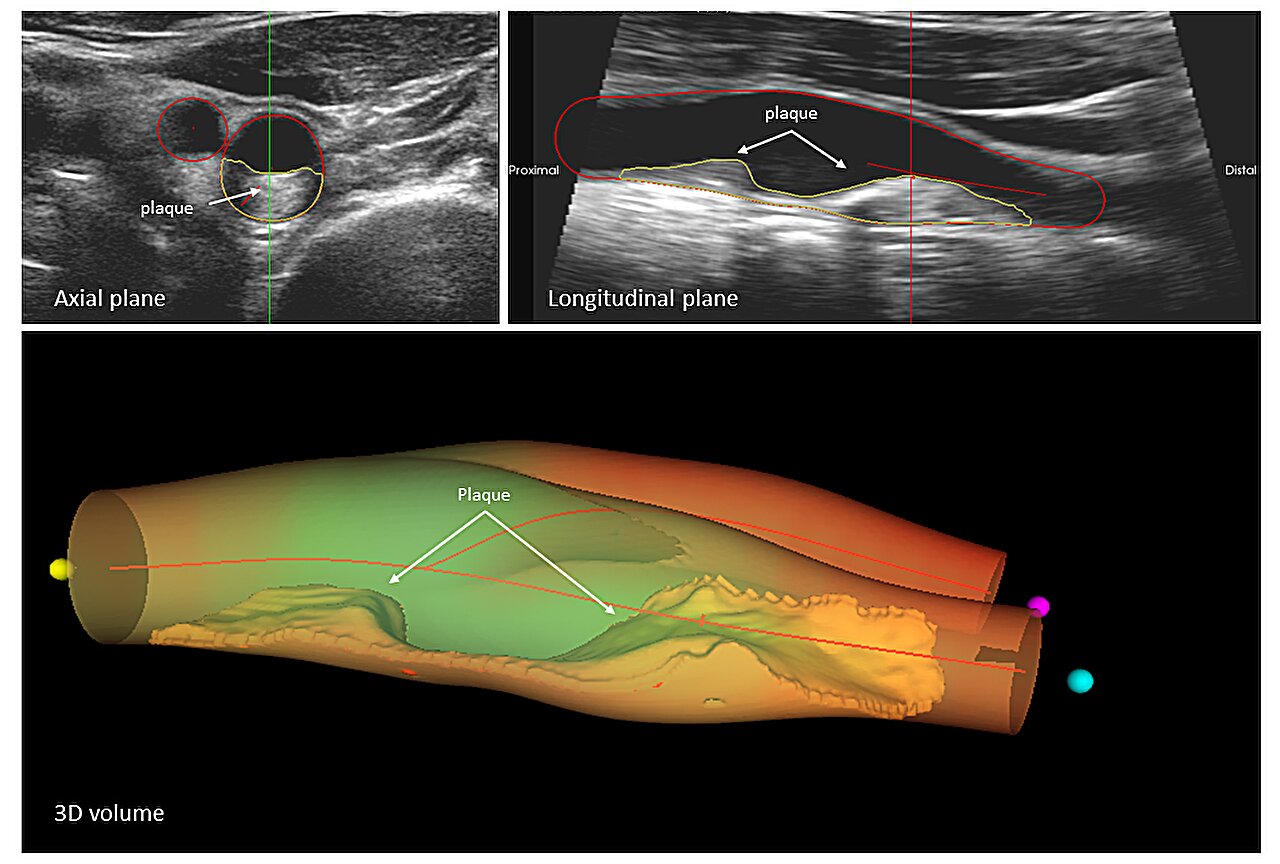
The BASHIR™ catheter is a small tube-like device that consists of a helical basket with six mini-infusion catheters at its farthest end. When the infusion basket is expanded within a clot in a large blood vessel, new channels open, enabling blood to flow through the clot. Blood that flows through carries the body’s clot-dissolving chemicals into the channels, accelerating clot breakdown. Researchers at THROMBOLEX™ Inc. were involved in developing and commercializing this platform technology.
The occlusion of small lung arteries is the major reason for the reduction in blood flow in patients with acute pulmonary embolism. “The more occlusions a patient has, the lower their survival,” Dr. Bashir said. “Among the treatment goals is relieving obstructions in both large and small arteries.”
Patients who survive may, over more extended periods, be at high risk of developing chronic thromboembolic pulmonary hypertension (CTEPH), which is a life-threatening condition caused by increased blood pressure in the lungs.
In the new study, Dr. Bashir and colleagues observed reductions in occlusions in segmental and proximal branches of the pulmonary artery 48 hours following treatment with the BASHIR™ catheter. The blockages decreased even in those arteries that were distant from where the infusion basket was located, enabling improved blood flow and healing of the right ventricle.
“We suspect that the improvements in blood flow are due to both the expansion of the basket and the flow of the body’s clot dissolving molecules into the clot, which cause the blockage to shrink,” Dr. Bashir said. “As the volume of blood flow improved, right ventricular function also improved, which could translate to better survival.”
In future work, Dr. Bashir and colleagues plan to investigate mechanisms behind the observed reductions in arterial blockage. More extensive trials are also needed to understand better the impact of treatment with the BASHIR™ catheter on patient survival and incidence of CTEPH.
Other researchers who contributed to the new study were Gregory Piazza, Division of Cardiovascular Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston; Brian Firth, Thrombolex Inc, New Britain, Pennsylvania; Kenneth Ouriel, NAMSA (SYNTACTX), New York; Akhilesh Sista, Division of Interventional Radiology, Department of Radiology, Cornell University School of Medicine, New York; Parth Rali, Department of Thoracic Medicine and Surgery, Lewis Katz School of Medicine, Temple University; Anthony Comerota, Inova Heart and Vascular Institute, Inova Alexandria Hospital, Alexandria, Virginia; Vladimir Lakhter, Division of Cardiovascular Diseases, Lewis Katz School of Medicine, Temple University; Ayman Iskander, Division of Cardiology, St Joseph’s Hospital, Syracuse; Malcolm Foster, Department of Cardiology, East Tennessee Heart, Turkey Creek, Knoxville; Ripal Gandhi, Division of Interventional Radiology, Miami Cardiac and Vascular Institute, Miami, Florida; Amir Darki, Department of Cardiology, Loyola University Medical Center, Maywood, Illinois; Robert Lookstein, Department of Radiology, Mount Sinai Hospital, New York; and Kenneth Rosenfield, Department of Cardiology, Massachusetts General Hospital, Boston.
Dr. Bashir is a co-founder and has an equity interest in Thrombolex, Inc., a medical device company developing interventional catheter-based therapies for the rapid and effective treatment of acute venous thromboembolic disorders. Temple University also holds financial interests in the BASHIR™ Endovascular Catheter and other Thrombolex products pursuant to the license granted to Thrombolex for the University’s interest in patents co-invented by Dr. Riyaz Bashir. As a result of these interests, Temple University could ultimately potentially benefit financially from the outcome of this research. These interests have been reviewed and approved by Temple University in accordance with its Institutional Conflict of Interest policy.