The time of day when blood is taken can affect the results of tests for diagnosing dementia, according to new research led by the University of Surrey. The study has been published in Translational Psychiatry.
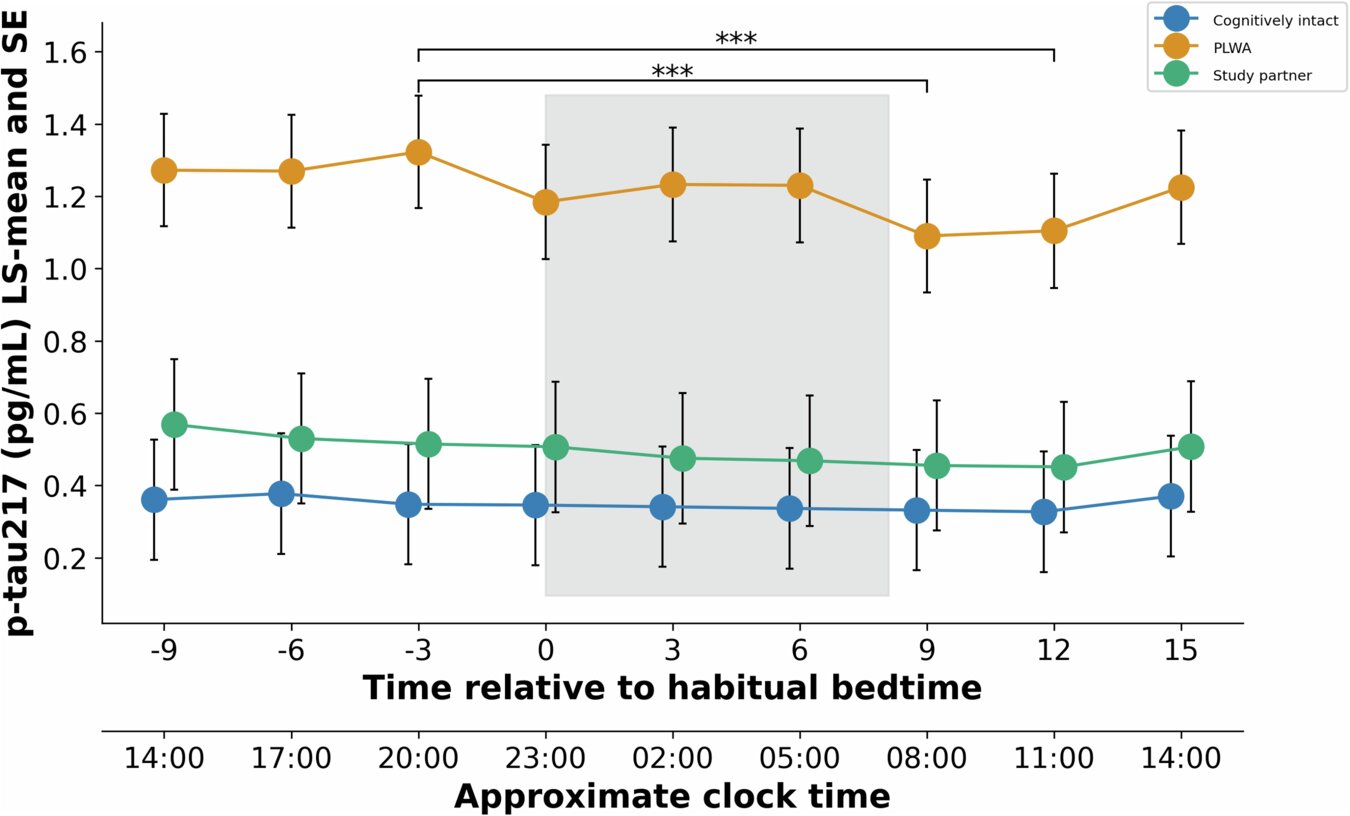
Researchers found that the biomarkers used to diagnose Alzheimer’s, including a promising marker for early diagnosis of the condition, varied significantly depending on the time of day. Biomarker levels were at their lowest in the morning when participants woke and highest in the evening.
The p-tau217 biomarker, which could help with early diagnosis of dementia, showed big differences depending on the time of day. Researchers discovered that the variation between morning and evening levels was similar to the changes seen in people whose mild memory problems get worse over a year.
Dr. Ciro della Monica, research fellow at the Surrey Sleep Research Centre at the University of Surrey and first author of the publication, said, “This work shows the importance of considering the time of day when taking clinical diagnostic samples and how the clinical picture for an individual may be affected by varying sample times. By standardizing the time of day that a sample is taken, the diagnosis of dementia and tracking disease progression can become more accurate.”
The study looked at 38 participants living with mild Alzheimer’s, their caregivers and health controls while they were residents at the Surrey Sleep Research Centre, which is part of the UK Dementia Research Institute’s (UK DRI) Care Research & Technology Centre.
Instead of taking one blood sample, as is the case in the majority of clinical practices, the participants had their blood taken every three hours for 24 hours. Four out of five measured biomarkers (p-tau217, Aβ40, Aβ42, and NfL) showed levels of fluctuation throughout the day. Only GFAP did not show a statistically significant variation.
Currently, it is not known what is driving these time-of-day differences. It may relate to sleep and sleep-related reduction in the production or clearance of these markers from the brain to the circulation, meals, posture, activity, or circadian mechanisms. Nevertheless, the findings imply that the time of day of sample collection is relevant in the implementation and interpretation of plasma biomarkers in dementia research and care. Overall, these findings indicate that the time of sampling should be standardized or at least recorded.
Professor Derk-Jan Dijk, Director of the Surrey Sleep Research Centre, UK DRI Group Leader and senior author of the publication, said, “Circadian rhythm research has demonstrated that almost all variables related to physiology and brain function vary with time of day. This study shows that translating this basic knowledge to the area of dementia research holds great promise for a better understanding, diagnosis and treatment of Alzheimer’s.”
More information:
Ciro della Monica et al, P-tau217 and other blood biomarkers of dementia: variation with time of day, Translational Psychiatry (2024). DOI: 10.1038/s41398-024-03084-7
Citation:
Dementia diagnostic markers shown to change with time of day (2024, October 2)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-dementia-diagnostic-markers-shown-day.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.