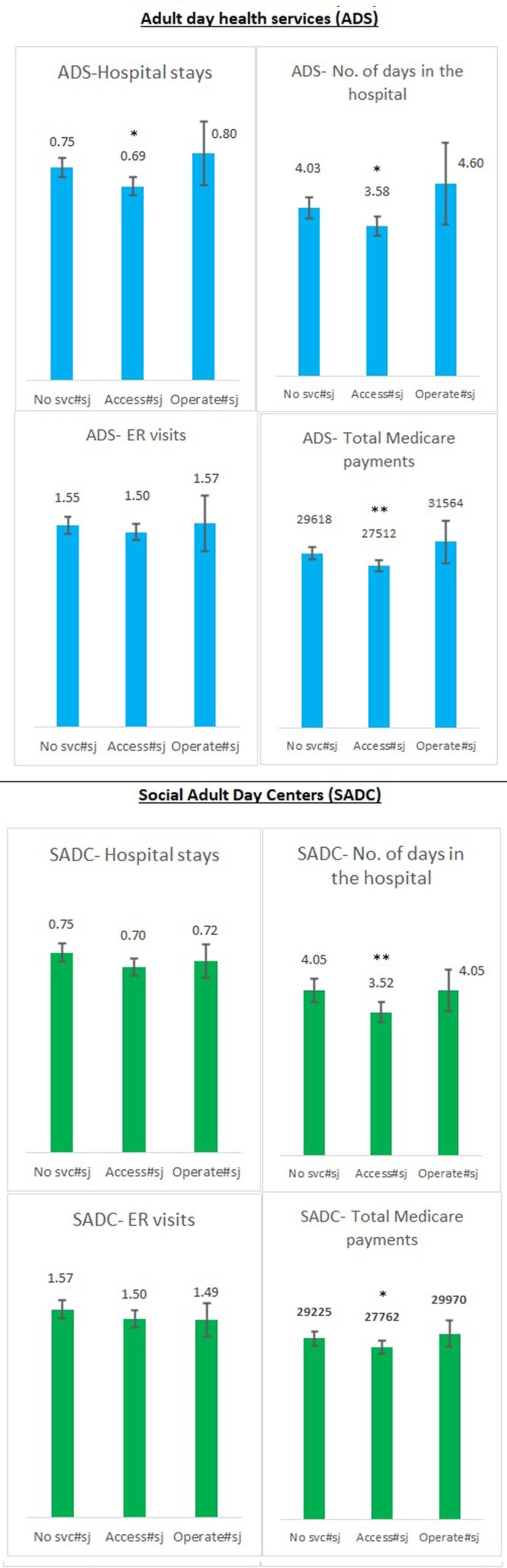
Living with dementia in communities with senior centers providing access to adult day health and social services was associated with fewer hospitalizations and lower health care use and Medicare costs, according to researchers from Rutgers University-New Brunswick and the University of Massachusetts Boston.
The results, published in Heath Affairs Scholar, underscore the potential of senior centers in minimizing health care costs and acute care usage among those with dementia, particularly in smaller communities where centers provide access to such services.
“Our findings provide evidence to support the growing interest in increasing funding for community-based organizations to improve health,” said Emily A. Greenfield, professor of social work and director of the Hub for Aging Collaboration at the Rutgers University School of Social Work. “Importantly, our work provides empirical evidence to support the recognition of senior centers as community-based assets with the potential to bring value to health care systems.”
Adult day health services offer specialized clinical care for community-dwelling older adults, including nursing services, health monitoring, medication administration, and occupational therapy. Social adult day services provide social and recreational activities in a supervised setting for people with mild to acute conditions. Unlike adult day health services, social adult day services aren’t licensed to provide clinical care.
The researchers said there is widespread agreement and interest among policymakers and practitioners about the role of community-based services in enhancing health outcomes among individuals living with dementia and their caregivers, though few studies have explored the impact of programming offered in senior centers on health outcomes among people living with dementia.
“In partnership with The Massachusetts Councils on Aging, we conducted a comprehensive assessment of the breadth and depth of the functions of councils on aging in our state,” said Caitlin Coyle, director of the Center for Social and Demographic Research on Aging at the University of Massachusetts Boston.
“Collecting data on organizational and programmatic characteristics of councils on aging—such as staffing, financing and types of services offered—can provide them with data to demonstrate their impact on the communities they serve.”
The study used data from the U.S. Centers for Medicare and Medicaid Services and data from the statewide census of the municipally based councils on aging and senior centers in Massachusetts. The sample included 48,474 adult residents with a diagnosis of dementia who were ages 75 years and older.
The researchers said Massachusetts is an ideal place to study the health system’s impact of such social care given that all but one of the 351 municipalities in Massachusetts have councils on aging—nearly synonymous with senior centers—that often provide dementia-focused programming.
Many of New Jersey’s municipalities also have senior centers, whose operations are largely funded by local and private investments. The researchers say the extent to which New Jersey senior centers offer adult day health and related services is unknown due to limited research on community-based aging organizations in the state.
Because these associations are correlational, the authors cannot conclude that one directly causes the other. But, considering the evidence in support of cost savings, the researchers said future research will help better understand the impact of dementia-focused programs offered through senior centers on the health care utilization of community-dwelling people living with dementia.
Ayse Akincigil, associate professor at the School of Social Work and health economist at the Rutgers Institute for Health, Health Care Policy and Aging Research of Rutgers, was lead author on the study. Co-authors include Divya Bhagianadh of University of Arkansas; Clara J. Scher, Emily A. Greenfield, and Natalie E. Pope of Rutgers University; and Ceara Somerville and Caitlin Coyle of University of Massachusetts Boston.
More information:
Ayse Akincigil et al, Dementia-focused programs in older adult centers and health care use among individuals with dementia, Health Affairs Scholar (2024). DOI: 10.1093/haschl/qxae108
Citation:
Community-based programs in senior centers may lower health care use and costs for people with dementia (2024, October 2)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-community-based-senior-centers-health.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.