Environmental phenols are found in a wide range of common consumer products. They include preservatives in packaged foods, parabens in shampoos and bisphenol A (BPA) in plastic dishware, so humans have broad exposure to them, day in and day out.
Some of these environmental phenols are known to have cardiac toxicities. Now, an interdisciplinary study involving four University of Cincinnati College of Medicine professors is revealing their adverse impact on the heart‘s electrical properties, and the research has been published in the journal Environmental Health.
“This is the first study to look at the impact of phenol exposure on cardiac electrical activity in humans,” said Hong-Sheng Wang, Ph.D., professor in the Department of Pharmacology, Physiology and Neurobiology and the study’s lead author.
Researchers used data from the Fernald Community Cohort, which includes nearly 10,000 people who lived near the former U.S. Department of Energy uranium processing site at Fernald, outside Cincinnati, and participated in the Fernald Medical Monitoring Program between 1990 and 2008.
Much of the cohort did not experience exposure to uranium beyond the radiation received by the general population. Wang and his team used their data, including biological samples and medical records, in the study so uranium exposure would not be a factor in the findings—making them relevant to the general population. Because urine samples and electrocardiograms, or EKGs, were collected on the same day, the results were significant for analyzing exposure to environmental phenols.
The EKGs, which measure cardiac electrical activities, were read by board-certified physicians, and the urine samples were sent to the Centers for Disease Control and Prevention for exposure analysis.
One goal of the study was to identify any changes in EKG parameters associated with environmental phenol exposure.
The heart is driven by electrical activity, so anything affecting its electrical properties can have a detrimental impact and possibly result in arrhythmias.
The research concluded higher exposure to some environmental phenols is associated with altered cardiac electrical activity.
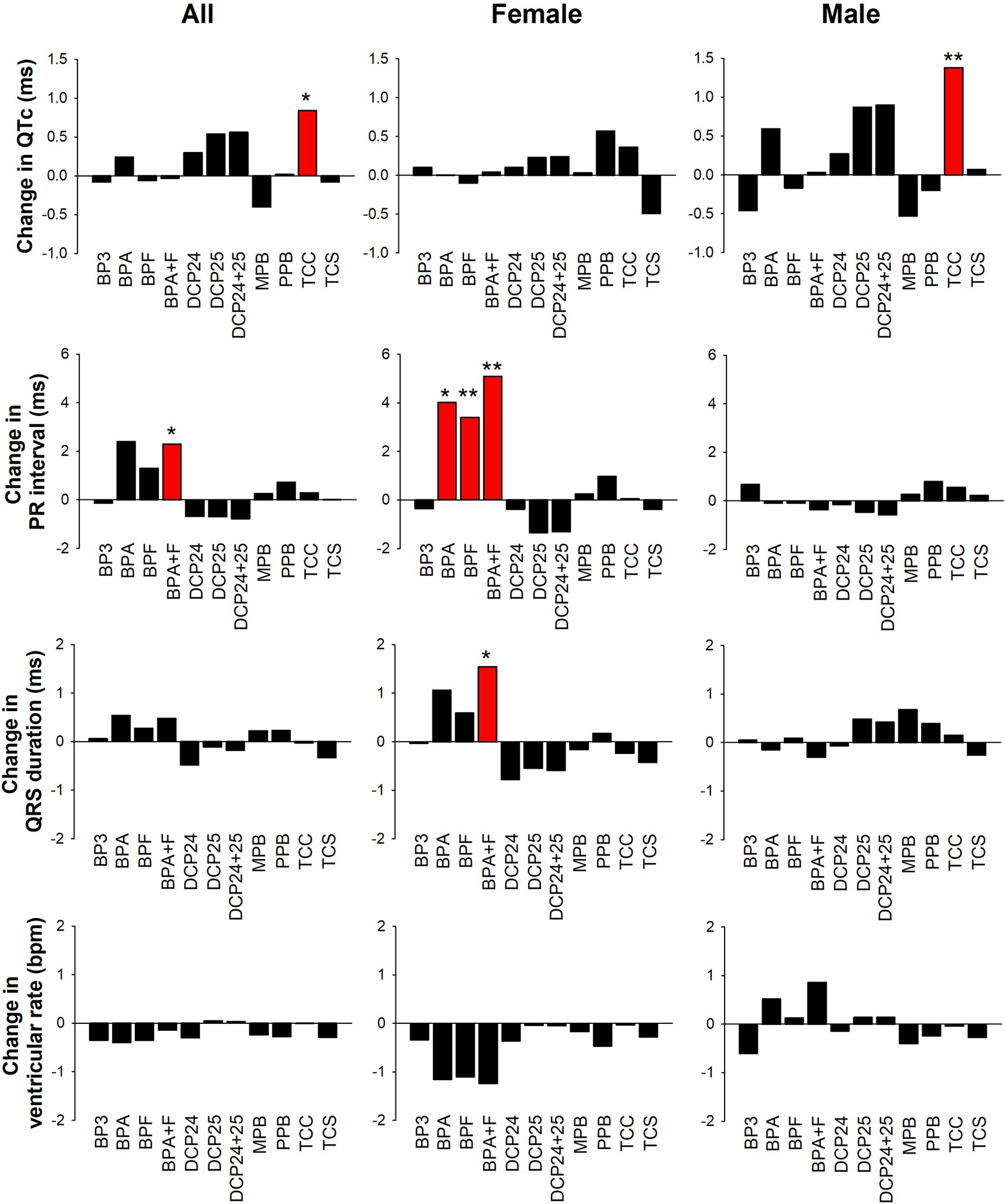
Researchers found that higher exposure to BPA, BPF and BPA+F in women is associated with a longer PR interval, a delay in the time it takes for electrical signals to move from the atria at the top of the heart to the ventricles.
“Our findings were highly sex-specific,” said Wang. In women, researchers identified an association with longer QRS duration, or contraction of the ventricles, and dysfunction of the electrical impulses of the heart.
“It was particularly pronounced in women with higher body mass indexes,” said Wang.
In men, researchers found higher exposure to triclocarban (TCC), an antimicrobial agent, led to longer QT intervals in the heart—meaning the heart’s electrical system is taking too long to recharge, a situation that can contribute to heart rhythm dysfunction. TCC has since been banned in the United States.
Wang also pointed out that typical exposure levels alone are unlikely to cause clinically significant heart disease in healthy people.
“These were not dramatic changes that we observed, but moderate changes to cardiac electrical activity,” he said. “However, they were particularly pronounced in certain subpopulations.”
He said the altered cardiac activity could exacerbate existing heart disease or arrhythmias in a patient, especially older adults or those with other risk factors.
“Now there are new chemicals out there, so the next step would be to examine these newer environmental chemicals and to focus on their impact on an individual level in those who are predisposed to heart disease,” said Wang.
Other contributors in this study included Susan Pinney, Ph.D., FACE, professor of epidemiology in the Department of Environmental and Public Health Sciences; Jack Rubinstein, MD, FACC, professor of clinical cardiology in the Department of Internal Medicine; and Changchun Xie, Ph.D., professor in the Department of Biostatistics, Health Informatics and Data Sciences.
More information:
Jack Rubinstein et al, Association of same-day urinary phenol levels and cardiac electrical alterations: analysis of the Fernald Community Cohort, Environmental Health (2024). DOI: 10.1186/s12940-024-01114-x
Citation:
Common consumer product chemicals now tied to cardiac electrical changes (2024, October 3)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-common-consumer-product-chemicals-cardiac.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.