Pain is a complex, multifaceted experience shaped by various factors beyond physical sensation, such as a person’s mindset and their expectations of pain. The placebo effect, the tendency for a person’s symptoms to improve in response to inactive treatment, is a well-known example of how expectations can significantly alter a person’s experience. Mindfulness meditation, which has been used for pain management in various cultures for centuries, has long been thought to work by activating the placebo response. However, scientists have now shown that this is not the case.
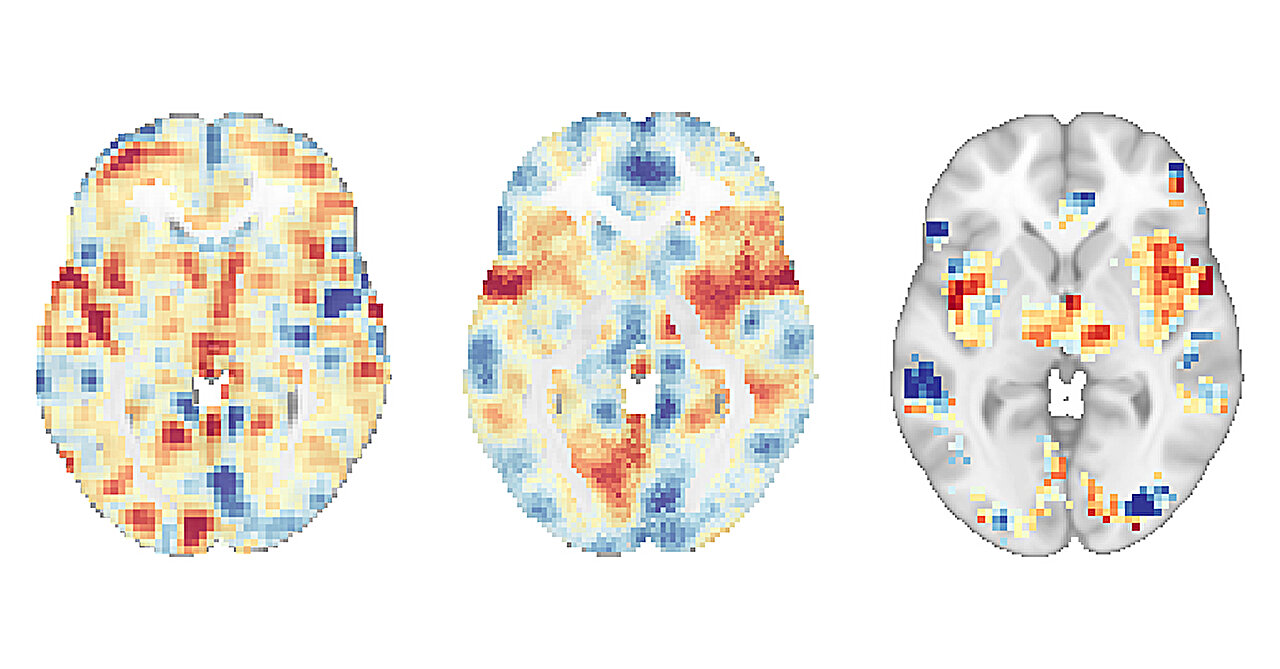
A new study, published in Biological Psychiatry, has revealed that mindfulness meditation engages distinct brain mechanisms to reduce pain compared to those of the placebo response. The study, conducted by researchers at University of California San Diego School of Medicine, used advanced brain imaging techniques to compare the pain-reducing effects of mindfulness meditation, a placebo cream and a “sham” mindfulness meditation in healthy participants.
The study found that mindfulness meditation produced significant reductions in pain intensity and pain unpleasantness ratings, and also reduced brain activity patterns associated with pain and negative emotions. In contrast, the placebo cream only reduced the brain activity pattern associated with the placebo effect, without affecting the person’s underlying experience of pain.
“The mind is extremely powerful, and we’re still working to understand how it can be harnessed for pain management,” said Fadel Zeidan, Ph.D., professor of anesthesiology and Endowed Professor in Empathy and Compassion Research at UC San Diego Sanford Institute for Empathy and Compassion. “By separating pain from the self and relinquishing evaluative judgment, mindfulness meditation is able to directly modify how we experience pain in a way that uses no drugs, costs nothing and can be practiced anywhere.”
The study included 115 participants, which consisted of two separate clinical trials in healthy participants, who were randomly placed into groups to be given four interventions: a guided mindfulness meditation, a sham-mindfulness meditation that only consisted of deep breathing, a placebo cream (petroleum jelly) that participants were trained to believe reduces pain, and as a control, one group listened to an audiobook. The researchers applied a very painful but harmless heat stimulus to the back of the leg and scanned the participants’ brains both before and after the interventions.
To analyze the participants’ brain activity patterns, the researchers used a novel approach called multivariate pattern analysis (MVPA), which uses machine learning to disentangle the many complex neural mechanisms underlying the experience of pain, including those stemming from specific heat stimuli, negative emotions and pain responses that are driven by the placebo effect. The researchers were then able to identify whether mindfulness meditation and placebo engage similar and/or separate brain processes.
Although placebo cream and sham-mindfulness meditation lowered pain, the researchers found that mindfulness meditation was significantly more effective at reducing pain when compared to placebo cream, sham-mindfulness meditation and the controls.
They also found that mindfulness-based pain relief reduced synchronization between brain areas involved in introspection, self-awareness and emotional regulation. These parts of the brain together comprise the neural pain signal (NPS), a documented pattern of brain activity thought to be common to pain in different individuals and different types of pain. In contrast, the placebo cream and sham-mindfulness meditation did not show a significant change in the NPS when compared to controls. Instead, these other interventions engaged entirely separate brain mechanisms with little overlap.
“It has long been assumed that the placebo effect overlaps with brain mechanisms triggered by active treatments, but these results suggest that when it comes to pain, this may not be the case,” said Zeidan. “Instead, these two brain responses are completely distinct, which supports the use of mindfulness meditation as a direct intervention for chronic pain rather than as a way to engage the placebo effect.”
In modern medicine, new therapies are generally deemed effective and reliable if they outperform placebo. As the present study found that mindfulness meditation is more powerful than placebo and does not engage the same neurobiological processes as placebo, the findings have important implications for the development of new treatments for chronic pain. However, it will take more research to demonstrate these effects in people living with chronic pain as opposed to healthy participants.
In the long term, the researchers hope that by understanding the distinct brain mechanisms underlying mindfulness meditation, they can design more effective and accessible interventions that harness the power of mindfulness to reduce pain in people with various health conditions.
“Millions of people are living with chronic pain every day, and there may be more these people can do to reduce their pain and improve their quality of life than we previously understood.” said Zeidan. “We are excited to continue exploring the neurobiology of mindfulness and how we can leverage this ancient practice in the clinic.”
Co-authors on the study include Gabriel Riegner and Jon Dean at UC San Diego School of Medicine and Tor Wager at Dartmouth College.
More information:
Gabriel Riegner et al, Mindfulness meditation and placebo modulate distinct multivariate neural signatures to reduce pain, Biological Psychiatry (2024). DOI: 10.1016/j.biopsych.2024.08.023
Citation:
Brain scans reveal that mindfulness meditation for pain is not a placebo (2024, September 5)
retrieved 6 September 2024
from https://medicalxpress.com/news/2024-09-brain-scans-reveal-mindfulness-meditation.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.