Babies born to pregnant women with obesity are more likely to develop heart problems and diabetes as adults due to fetal damage caused by the high-fat, high-energy diet of their mother.
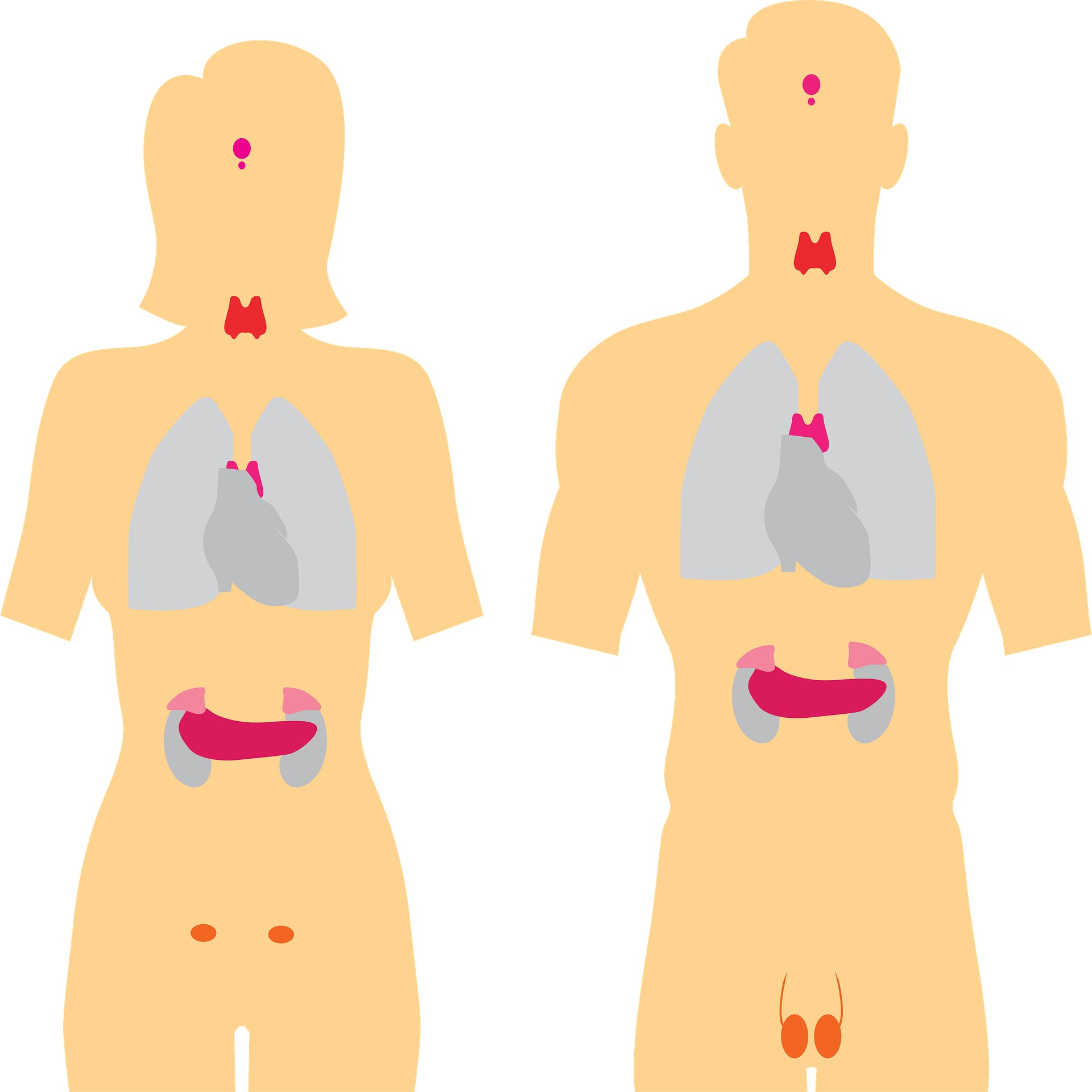
That’s the groundbreaking finding from a new study published in the Journal of Physiology that shows for the first time that maternal obesity alters a critical thyroid hormone in the fetal heart, disrupting its development.
Consuming a high-fat, sugary diet during pregnancy also increases the likelihood of the unborn baby becoming insulin resistant in adulthood, potentially triggering diabetes and causing cardiovascular disease. This is despite babies being a normal weight at birth.
University of South Australia researchers identified the link by analysing tissue samples from the fetuses of pregnant baboons fed a high-fat, high-energy diet in a biomedical research institute in the United States. They then compared this to fetuses from baboons on a control diet.
Lead author, University of South Australia PhD candidate Melanie Bertossa, says the findings are significant because they demonstrate a clear link between an unhealthy diet high in saturated fats and sugar, and poor cardiovascular health.
“There has been a long-standing debate as to whether high-fat diets induce a hyper- or hypothyroid state in the fetal heart. Our evidence points to the latter,” Bertossa says.
“We found that a maternal high-fat, high-energy diet reduced concentrations of the active thyroid hormone T3, which acts like a switch around late gestation, telling the fetal heart to start preparing for life after birth. Without this signal, the fetal heart develops differently.”
Bertossa says that diets high in fat and sugar can alter the molecular pathways involved in insulin signalling and critical proteins involved in glucose uptake in the fetal heart. This increases the risk of cardiac insulin resistance, often leading to diabetes in adulthood.
“You’re born with all the heart cells you will ever have. The heart doesn’t make enough new heart muscle cells after birth to repair any damage, so changes that negatively impact these cells before birth could persist for a lifetime.
“These permanent changes could cause a further decline in heart health once children reach adolescence and adulthood when the heart starts to age.”
Senior author, UniSA Professor of Physiology Janna Morrison, says the study demonstrates the importance of good maternal nutrition in the leadup to pregnancy, not only for the mother’s sake but also for the health of the baby.
“Poor cardiac outcomes were seen in babies that had a normal birth weight — a sign that should guide future clinical practice,” Prof Morrison says.
“Cardiometabolic health screening should be performed on all babies born from these types of pregnancies, not just those born too small or too large, with the goal being to detect heart disease risks earlier.”
Prof Morrison says that if rising rates of high-fat sugary diets are not addressed, more people will develop health complications such as diabetes and cardiovascular disease, which could result in shorter life spans in the decades ahead.
“Hopefully, with the knowledge we have now about the negative health impacts of obesity, there is potential to change this trajectory.”
The researchers are currently undertaking long-term studies of babies born to women on high- fat high-energy diets to track their health over decades.