People with diabetes take insulin to lower high blood sugar. However, if glucose levels plunge too low—from taking too much insulin or not eating enough sugar—people can experience hypoglycemia, which can lead to dizziness, cognitive impairment, seizures or comas. To prevent and treat this condition, researchers in ACS Central Science report encapsulating the hormone glucagon. In mouse trials, the nanocapsules activated when blood sugar levels dropped dangerously low and quickly restored glucose levels.
Glucagon is a hormone that signals the liver to release glucose into the bloodstream. It’s typically given by injection to counteract severe hypoglycemia in people who have diabetes. While an emergency glucagon injection can correct blood sugar levels in about 30 minutes, formulations can be unstable and insoluble in water. In some cases, the hormone quickly breaks down when mixed for injections and clumps together to form toxic fibrils. Additionally, many hypoglycemic episodes occur at night, when people with diabetes aren’t likely to test their blood sugar.
To improve commercial glucagon stability and prevent hypoglycemia, researchers Andrea Hevener and Heather Maynard looked to micelles: nanoscale, soap-like bubbles that can be customized to assemble or disassemble in different environments and are used for drug delivery.
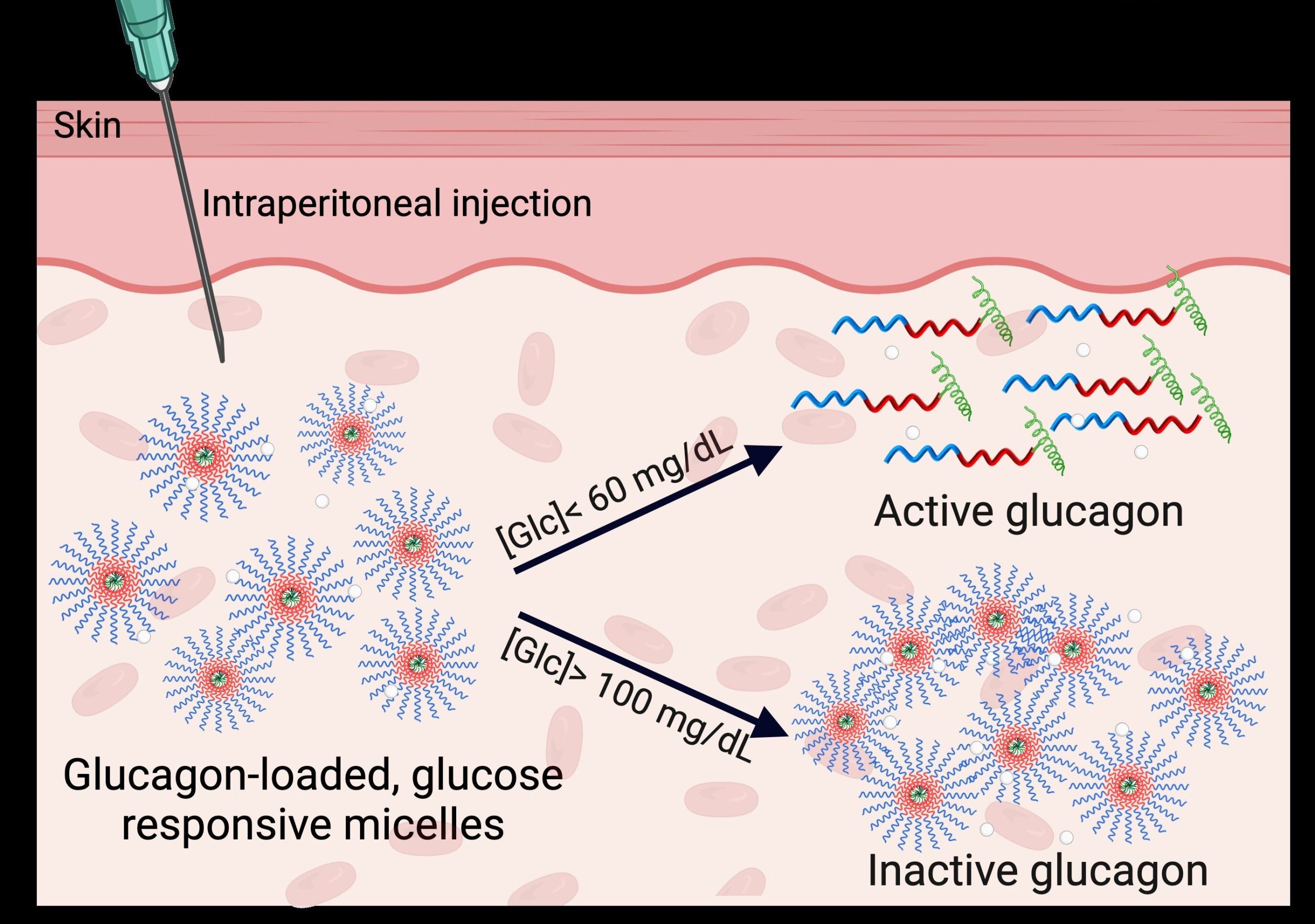
They developed a glucose-responsive micelle that encapsulates and protects glucagon in the bloodstream when sugar levels are normal but dissolves if levels drop dangerously low. To prevent hypoglycemia, the micelles could be injected ahead of time and circulate in the bloodstream until they are needed.
In lab experiments, the researchers observed that the micelles disassembled only in liquid environments that mimicked hypoglycemic conditions in both human and mice bodies: less than 60 milligrams of glucose per deciliter. Next, when mice experiencing insulin-induced hypoglycemia received an injection of the specialized micelles, they achieved normal blood sugar levels within 40 minutes.
The team also determined that glucagon-packed micelles stayed intact in mice and didn’t release the hormone unless blood glucose levels fell below the clinical threshold for severe hypoglycemia. From additional toxicity and biosafety studies in mice, the researchers note that empty micelles didn’t trigger an immune response or induce organ damage.
While more studies are needed, the researchers say their proof-of-concept is a first step toward a new on-demand and effective method for preventing or mitigating extremely low blood sugar levels.
More information:
A Glucose-Responsive Glucagon-Micelle for the Prevention of Hypoglycemia, ACS Central Science (2024). DOI: 10.1021/acscentsci.4c00937
Citation:
A new injectable shows promise to prevent and treat hypoglycemia (2024, October 2)
retrieved 5 October 2024
from https://medicalxpress.com/news/2024-10-hypoglycemia.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.