Researchers at the University of Pittsburgh are pioneering a new approach to blood pressure monitoring—using the devices we carry with us every day.
Ramakrishna Mukkamala, professor of bioengineering at Pitt’s Swanson School of Engineering, is passionate about developing accessible blood pressure (BP) detection tools. Instead of designing a new medical device to monitor BP, Mukkamala decided to take advantage of what is in nearly everyone’s pockets—smartphones—and figure out how to detect blood pressure using sensors already built into them.
“The most significant thing you can do to reduce your risk of cardiovascular disease is to lower high blood pressure through lifestyle changes, but in underserved populations, many people don’t have access to blood pressure cuffs, regular doctor’s appointments, or even know it’s a problem,” Mukkamala said. “But they do have smartphones.”
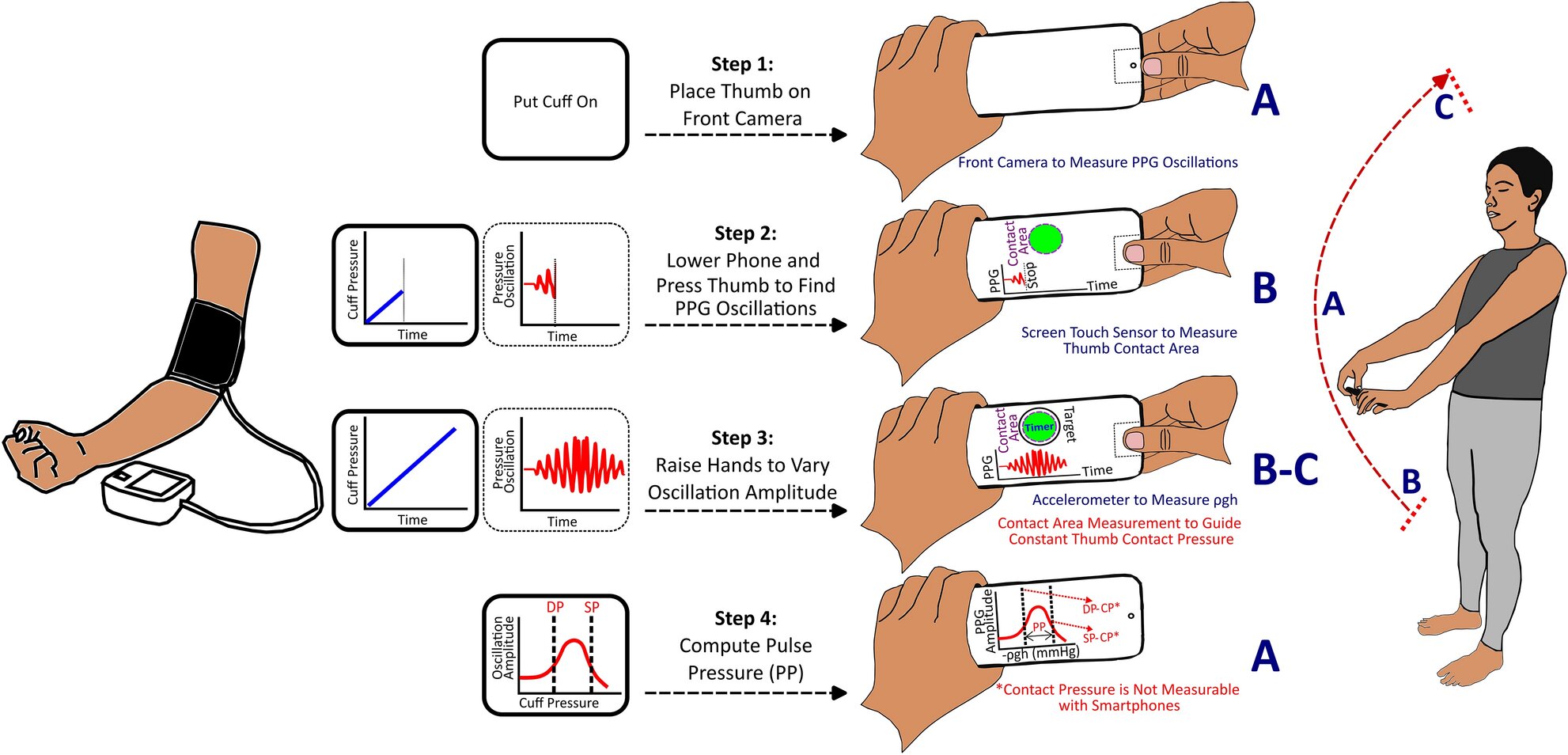
Mukkamala’s team harnessed tools already built into most smartphones, like motion-sensing accelerometers, front cameras, and touch sensors to build a smartphone application on an Android that can measure an individual’s pulse pressure. The user performs a hand-raising motion while holding the smartphone to make a measurement. The results of the project “A smartphone application toward detection of systolic hypertension in underserved populations” published in Scientific Reports, demonstrate a promising new technology that could uniquely help reduce the burden of systolic hypertension globally, particularly in underserved populations.
Designing blood pressure technology for a touchscreen
Turning a smartphone into a monitoring device is no easy task, as Vishaal Dhamotharan, graduate student in the Cardiovascular Health Tech Laboratory, found out through multiple iterations of app development. Because smartphones don’t have force sensing tools, a crucial element of the project was figuring out how to replicate the effects of a traditional blood pressure exam using only a cell phone, which the team solved by using a familiar force—gravity.
“Because of gravity, there’s a hydrostatic pressure change in your thumb when you raise your hands up above your heart, and using the phone’s accelerometer, you’re able to convert that into the relative change in pressure,” Dhamotharan said.
By pairing this hand-raising motion with guided thumb maneuvers on the smartphone, the team was able to calculate each participant’s pulse pressure. Pulse pressure is the difference between your upper (systolic) and lower (diastolic) numbers—for example, an individual with a BP measurement of 120/80 has a pulse pressure of 40. For Sanjeev Shroff, collaborator and bioengineering department chair, this publication is a promising advancement for blood pressure measurement devices.
“Development of a cuffless blood pressure measurement device that does not require any external calibration is the holy grail—such a device currently does not exist,” Shroff said. “The research work reported in this publication is an important step in the right direction, and is also encouraging for additional work aimed at obtaining systolic, diastolic, and mean pressures.”
Although pulse pressure isn’t typically used in cardiovascular disease monitoring, the study revealed its significance as a metric for detecting hypertension, according to Céderick Landry, assistant professor at the University of Sherbrooke and former postdoctoral researcher in the lab.
“Guidelines typically require doctors to measure both systolic and diastolic blood pressure, and pulse pressure is just the difference between the two,” Landry said. “We showed that if you only have access to pulse pressure, it’s still very correlated with hypertension, so part of our challenge now is changing the mentality on how to best measure things.”
Hypertension management within reach
Systolic hypertension, or high blood pressure, affects more than 4 billion adults worldwide and is the leading modifiable risk factor for cardiovascular disease, the top cause of death globally. This app could bring blood pressure monitoring software to any smartphone owner, enabling consistent self-monitoring and easy sharing of results with health care providers. This innovation is especially promising for managing hypertension, which can often be lowered through lifestyle changes such as reducing salt intake, quitting smoking and exercising regularly.
“This app would be really useful in low-income settings where people may not even have existing access to blood pressure tools,” Dhamotharan said. “Being able to measure blood pressure more frequently would allow an individual to track any significant changes in blood pressure, monitor for hypertension, and be able to manage their conditions with that knowledge.”
With people living in rural parts of the U.S. 40% more likely than urban residents to develop heart disease, this technology could be crucial for providing accessible health care tools to communities both in the United States and around the globe. Looking ahead, Mukkamala’s team is working on further improving smartphone blood pressure monitoring to the point that it can get in the hands of the people who need it most.
“The research is here—we just need some help making the technology better,” Landry said. “This is the first method of its kind, and even better, it’s something that we can start implementing right now.”
More information:
Cederick Landry et al, A smartphone application toward detection of systolic hypertension in underserved populations, Scientific Reports (2024). DOI: 10.1038/s41598-024-65269-w
Citation:
A new app uses smartphone technology to ‘uncuff’ blood pressure monitoring (2024, September 12)
retrieved 13 September 2024
from https://medicalxpress.com/news/2024-09-app-smartphone-technology-uncuff-blood.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.