Measuring levels of key proteins in patients’ saliva may be a relatively easy way for dentists and even patients themselves to track the progression of gum disease (periodontitis), suggests a new study led by researchers at Penn Dental Medicine.
In the study, the researchers monitored and tested saliva samples from more than 400 patients for up to a year and a half. They found that on average, patients who experienced progression of periodontitis showed substantially more elevated levels of nine inflammation-related signaling proteins in saliva when compared to those that did not.
The study is published in the December special issue of the Journal of Clinical Periodontology.
“One can imagine a saliva test kit, based on such findings, that dentists could use and even periodontitis patients could use at home—it could be a very useful personalized-dentistry tool for assessing risk and tailoring care delivery,” says study lead author Flavia Teles, DDS, MS, DMSc, Associate Professor in the Department of Basic & Translational Sciences at Penn Dental Medicine.
Periodontitis is one of the most common medical conditions, with an estimated prevalence of between 20% and 50% of the global population, including about 64 million people in the U.S. If untreated, this chronic bacterial infection and inflammation of the gums often leads to the loss of the bone that anchors teeth, which can then cause tooth loss.
Researchers haven’t had a good way to predict periodontitis progression from a mild state to one that is more severe and threatens tooth loss. In principle, periodic testing of saliva and/or blood samples might yield molecular clues.
However, prior studies of this strategy have had significant limitations, including small numbers of patients enrolled, small numbers of molecules measured, and the taking of samples at just one time-point instead of over a long interval. Teles’s new study was designed to surmount those limitations.
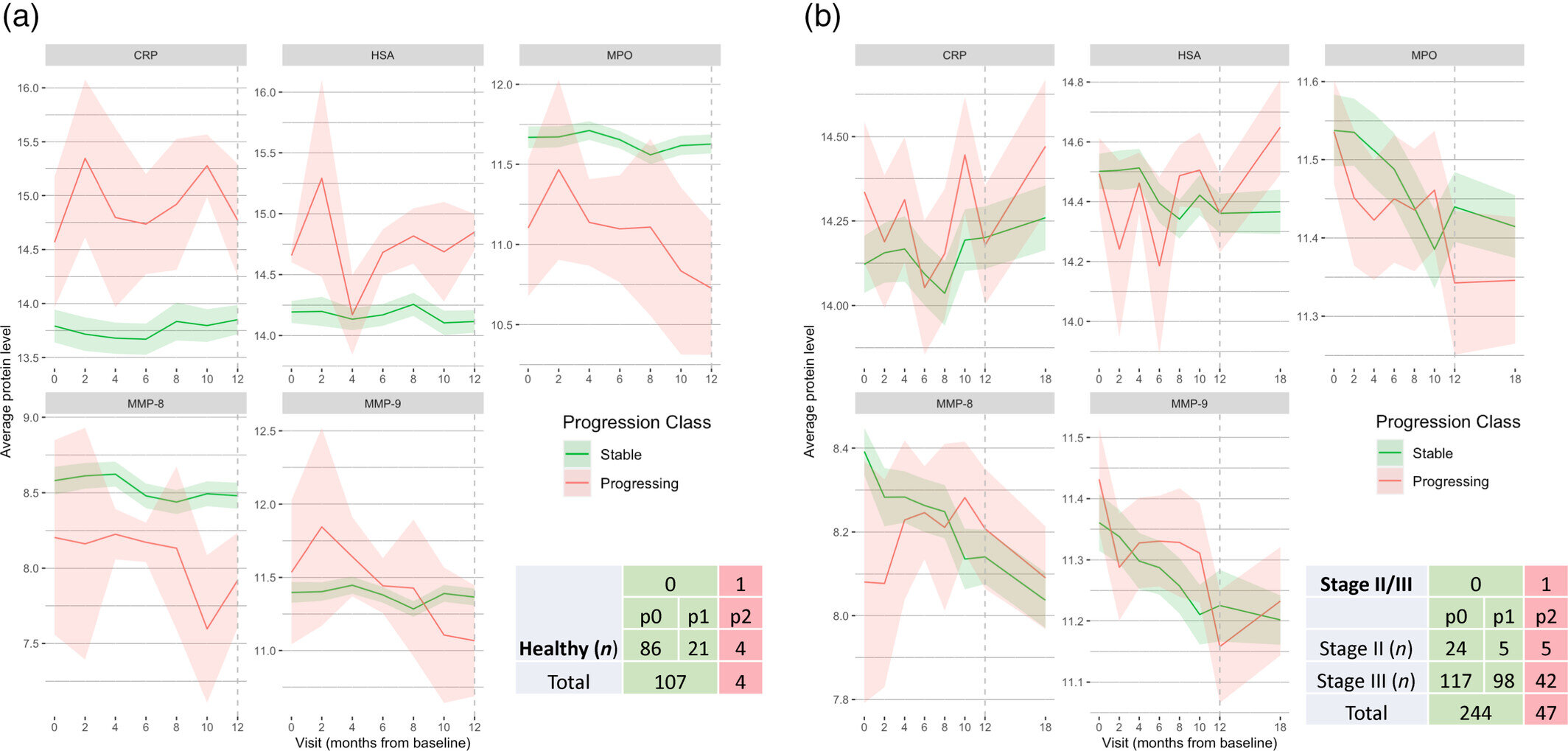
The researchers enrolled 302 individuals who had signs of early to moderate/severe periodontitis, and 113 individuals without periodontitis signs. Each subject received a detailed checkup with standard assessments of periodontitis status and progression every two months for a year.
Subjects also had saliva and blood samples taken at each checkup; the saliva samples were tested for levels of 10 different inflammation-linked proteins, and the blood samples for 5 different inflammatory proteins. When the year was up, researchers gave the periodontitis subjects standard non-surgical periodontal therapy and checked them again three and six months later.
The results showed that periodontitis patients who had the most disease progression during the year—defined as three or more sites with loss of clinical attachment (i.e., loss of fibers that help maintain the tooth in place)—had significantly higher levels of several inflammation-related signaling proteins in their saliva samples. These included interferon-gamma, IL-6, VEGF, IL-1β and MMP-8. Following treatment, these levels subsided.
The levels of such proteins in subjects’ blood did not differ significantly by degree of disease progression, although several, including MMP-8, MMP-9, and C-reactive protein, did fall significantly following treatment.
The findings suggest that changes in levels of inflammation-related proteins in saliva over time can help patients and doctors assess the risk of periodontitis progression as well as the effectiveness of treatment—and that blood levels also may be helpful in the latter case.
Teles and her colleagues in follow-on research are analyzing, in samples from the same patients, bacterial species and related small molecules called metabolites, to see if these too can help in tracking periodontitis status.
“We are also using artificial intelligence to analyze more broadly broader sets of clinical and laboratorial data,” says Teles, who was the inaugural recipient of the Artificial Intelligence in Oral Health Innovation Award, presented by the School’s Center for Innovation & Precision Dentistry (CiPD) and Penn’s Institute of Biomedical Informatics earlier this year.
“Our hope is that through this data analysis, we can further refine this approach and provide more tailored and accessible oral care.”
More information:
Flavia R. F. Teles et al, Salivary and serum inflammatory biomarkers during periodontitis progression and after treatment, Journal of Clinical Periodontology (2024). DOI: 10.1111/jcpe.14048
Citation:
Saliva proteins linked to gum disease progression identified (2025, January 8)
retrieved 8 January 2025
from https://medicalxpress.com/news/2025-01-saliva-proteins-linked-gum-disease.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.