A study from the Karolinska Institutet, published in Science Translational Medicine, shows that people with type 2 diabetes have lower levels of the protein that breaks down and converts creatine in the muscles. This leads to impaired function of the mitochondria, the ‘powerhouses’ of the cell.
Creatine is a natural compound in the body that is also found in foods such as meat and fish. It is also a popular supplement for improving exercise performance as it can make muscles work harder and longer before they become fatigued.
Despite creatine’s recognized positive effects, previous studies have suggested a possible link between high blood creatine levels and an increased risk of type 2 diabetes. This has raised questions about whether creatine supplementation may contribute to that risk.
New research based on studies in both humans and mice shows that people with type 2 diabetes have lower protein levels in their muscles that metabolizes and converts creatine—a protein called creatine kinase.
“This reduced protein level leads to impaired creatine metabolism in the muscle. This may explain why people with type 2 diabetes accumulate creatine in their blood,” says Anna Krook, Professor at the Department of Physiology and Pharmacology at Karolinska Institutet and the study’s principal investigator.
Scientists don’t know exactly what high creatine levels in the blood mean for the body, but it is known that it does have an effect outside the cells.
“The findings indicate that impaired creatine metabolism is a consequence of type 2 diabetes, rather than a cause of the disease,” says Krook.
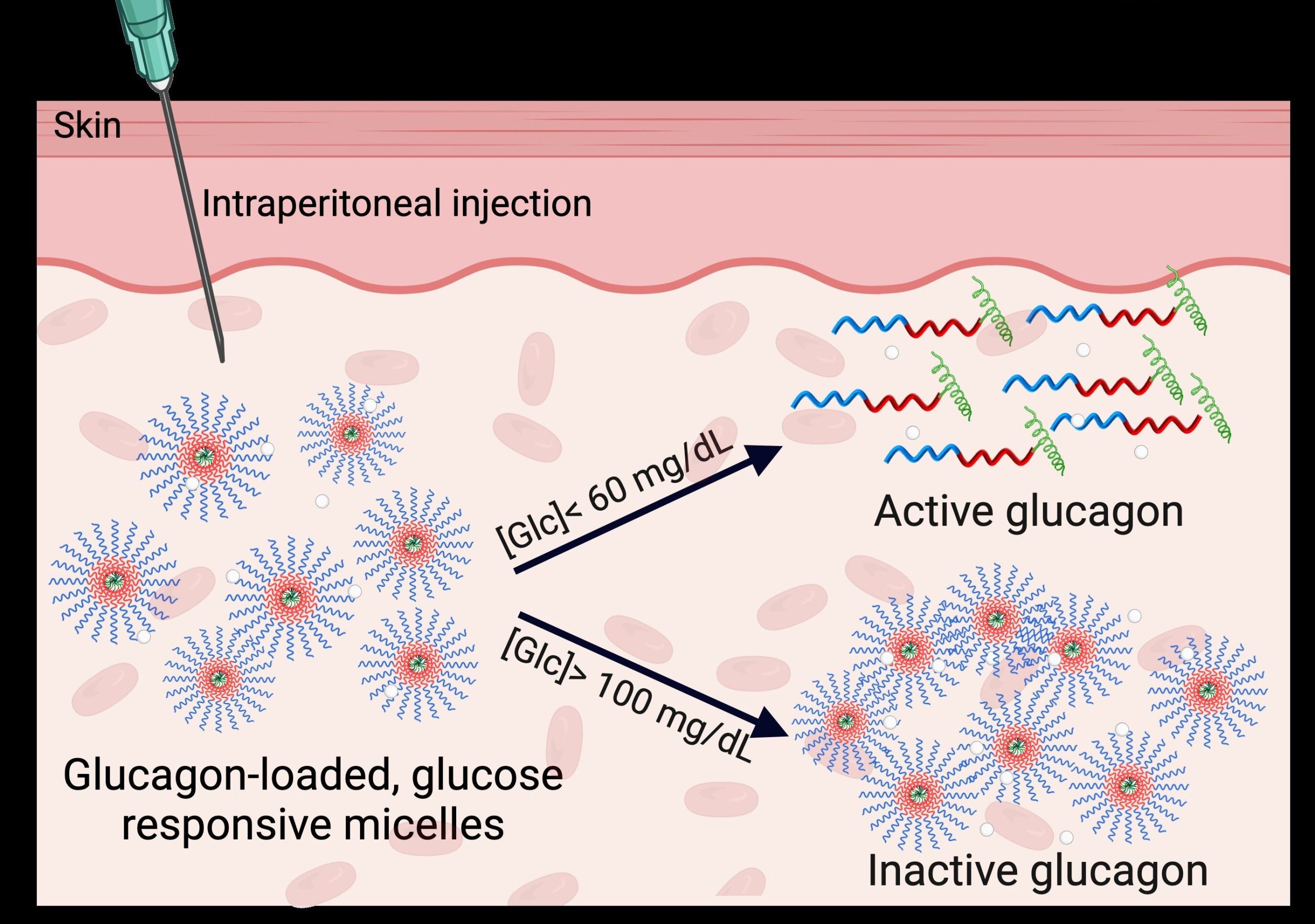
The study also shows that low levels of creatine kinase are not only linked to higher creatine levels in the blood, but also impair the function of mitochondria in the muscle. Mitochondria, which convert nutrients into energy, function less well in muscle cells with reduced creatine kinase, leading to both lower energy production and increased cell stress.
“This is quite consistent with the fact that people with type 2 diabetes have poorer energy metabolism. In the future, one possibility could be to regulate creatine kinase as part of the treatment of metabolic diseases such as obesity and diabetes,” says Krook.
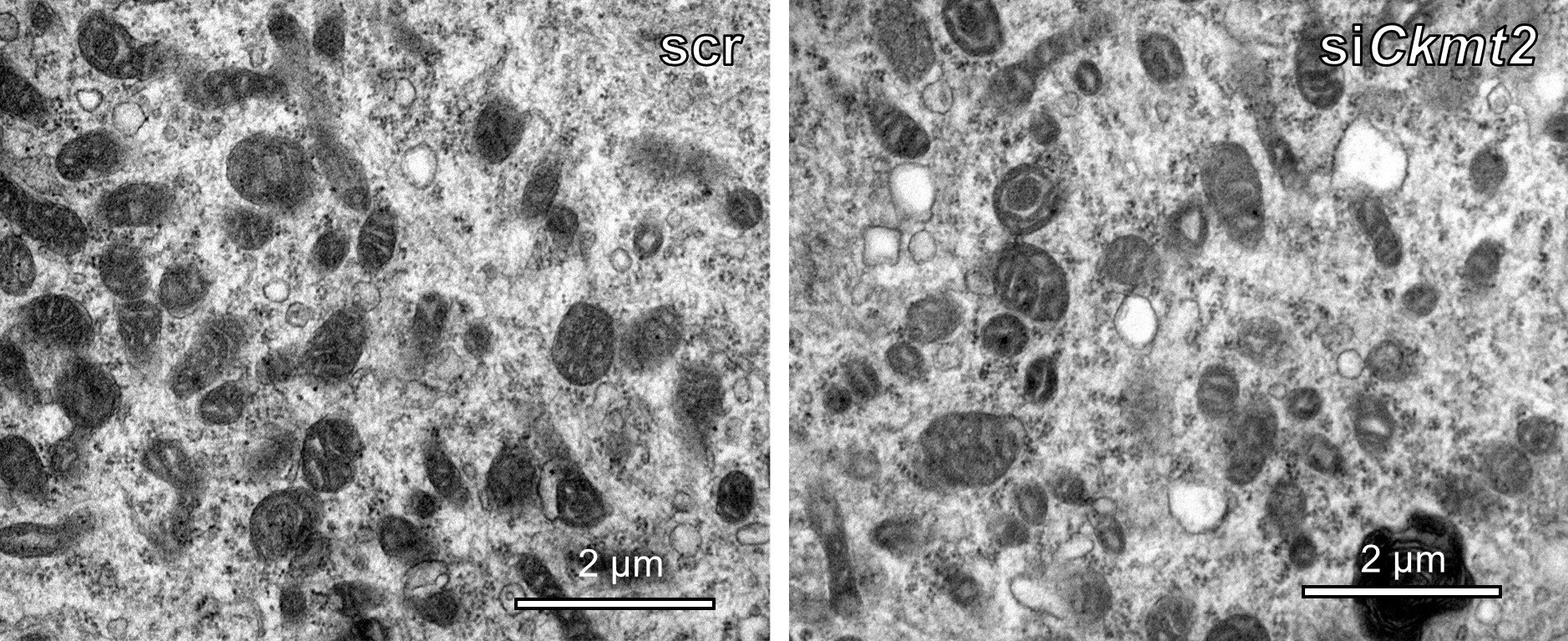
An unexpected finding of the study was that changes in creatine kinase levels affected the appearance of mitochondria and also their ability to produce energy, regardless of the amount of creatine available.
“This suggests that although the main role of creatine kinase is to process creatine, it affects mitochondrial function in other ways,” explains David Rizo-Roca, the study’s first author.
“Our next step is to find the molecular mechanisms behind these effects,” he says.
More information:
David Rizo-Roca et al, Decreased mitochondrial creatine kinase 2 impairs skeletal muscle mitochondrial function independently of insulin in type 2 diabetes, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.ado3022. www.science.org/doi/10.1126/scitranslmed.ado3022
Citation:
Study shows how muscle energy production is impaired in type 2 diabetes (2024, October 9)
retrieved 16 October 2024
from https://medicalxpress.com/news/2024-10-muscle-energy-production-impaired-diabetes.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.