Tumor vaccines can help the body fight cancer. These vaccines alert the patient’s immune system to proteins that are carrying cancer-typical alterations. Physicians and cancer researchers from Heidelberg and Mannheim have now treated adult patients with advanced midline gliomas, difficult-to-treat brain tumors, with a peptide vaccine for the first time. The vaccine mimicked a mutational change in a histone protein typical of this type of cancer. The vaccine proved to be safe and induced the desired immune responses directed against the brain tumor.
Crucial for the success of cancer vaccinations are protein structures by which the immune cells can recognize the cancer — and which are not present (or only to a small extent) on healthy cells. Mutations in the tumor genome often lead to protein structures that are altered in a way typical of cancer.
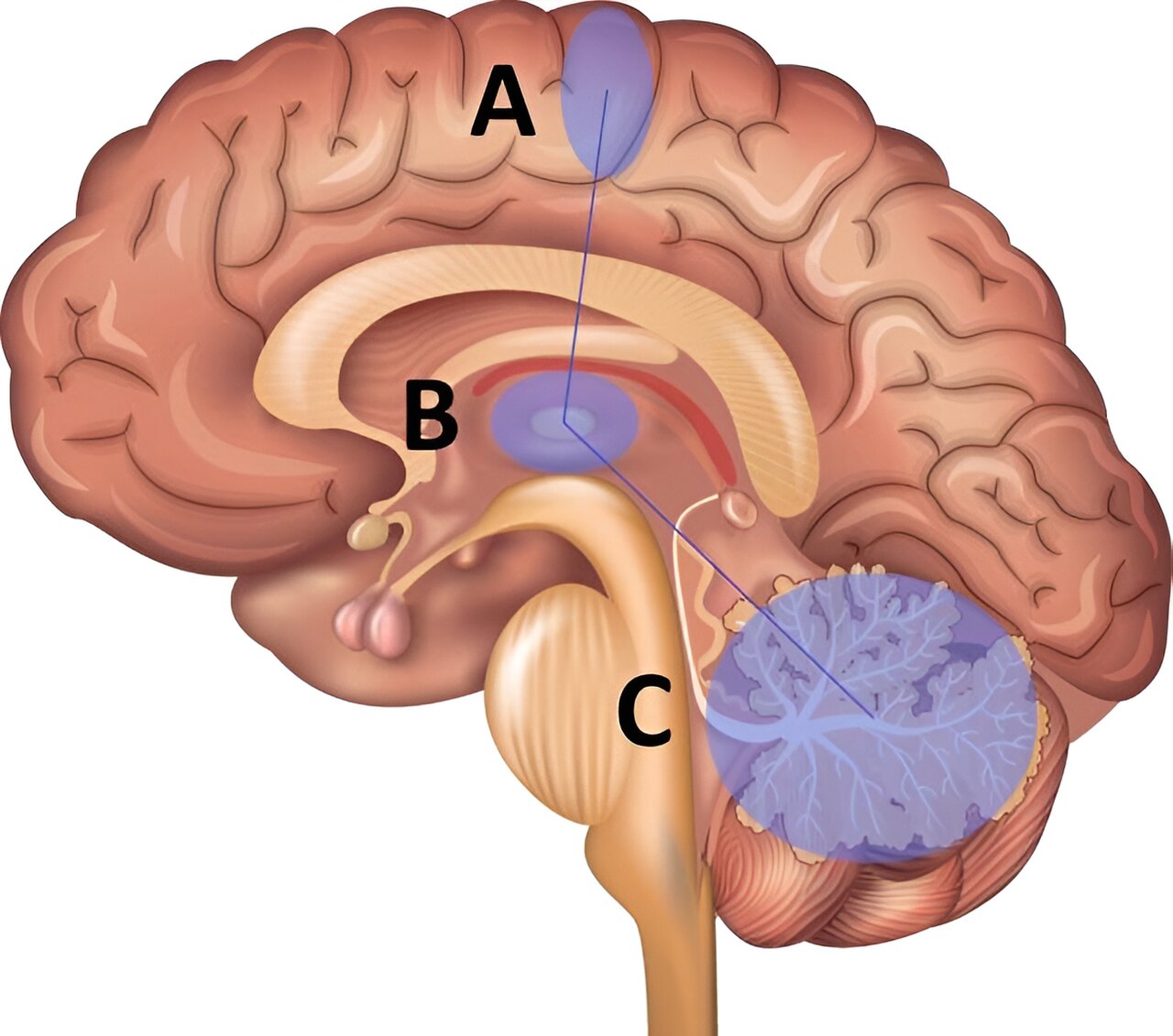
Diffuse midline gliomas are among the most aggressive brain tumors. They usually occur in children and young adults near the brain stem and are therefore difficult to access surgically. Chemotherapy or radiation therapy also have limited effectiveness. In this type of cancer, mutations characteristically occur in the gene encoding histone H3 (H3K27M), a packaging protein of DNA. The mutation gives rise to a novel protein structure — a so-called neoepitope — that can be recognized as foreign by the patient’s immune system.
“Such mutations, which occur in identical form in many patients, are rare in cancer. They literally lend themselves to the development of tumor vaccines because they occur in all cancer cells, since the mutated histone is causative for the development of midline gliomas. This means that vaccination against the mutated protein gets to the root of the problem,” explains Michael Platten, Director of the Department of Neurology at the University Medical Center Mannheim and Head of Department at the German Cancer Research Center (DKFZ).
The researchers led by Katharina Sahm and Michael Platten synthetically reconstructed the section of the histone H3 protein with the characteristic mutation. Using this peptide, they were able to curb the growth of H3K27M-mutated tumors in a mouse model. Encouraged by the results, the team decided to test the mutation-specific vaccine produced at the University of Tübingen in patients in a phase I-trial*, which is still ongoing.
In parallel, the physicians, together with colleagues from Munich, Berlin, Bonn and Münster, treated eight adult patients with the peptide vaccine in time-limited individual curative trials. These patients, who could not be enrolled in the trial protocol, suffered from diffuse midline gliomas with H3K27M mutation that progressed after standard therapy. Some of the affected individuals received therapy with immune checkpoint inhibitors in addition to tumor vaccination.
No serious side effects were observed in any of the vaccinated patients. Five of the eight treated patients developed specific immune responses against the mutant protein, which were dominated by CD4 T-helper cells. In one of the patients who had shown a strong immune response, the tumor regressed completely and she remained tumor-free for 31 months.
The vaccine peptide, which is comparatively long at 27 amino acids, worked in patients with different HLA variants. HLA proteins are responsible for the presentation of the mutant peptide on the cell surface and differ from person to person depending on their genetic background. Supported by the HI-TRON Mainz — Helmholtz Institute of the DKFZ, the researchers also observed that immune responses decreased over time, so repeated administration of the vaccine could support a sustained effect.
“We cannot make any further statements about the efficacy of the vaccination based on these treatments. In any case, the current study has given us valuable information that will help us to further optimize the development of brain tumor vaccines in the future,” explains the study’s senior author Katharina Sahm, senior physician at the Neurological University Hospital Mannheim and DKFZ researcher. A phase I-trial is currently underway to test the vaccine against the H3K27M mutation in patients with newly diagnosed midline gliomas. Evaluation is expected to begin around 2025.
The project was funded by the Translational Oncology funding program of German Cancer Aid (Deutsche Krebshilfe).
* INTERCEPT-H3 trial: https://classic.clinicaltrials.gov/ct2/show/NCT04808245