Houston Methodist researchers have discovered a more accurate and timely way to deliver life-saving drug therapies to the brain, laying the groundwork for more effective treatment of brain tumors and other neurological diseases.
In a study published this month in Communications Biology, an open access journal from Nature Portfolio, investigators used an electric field to infuse medicine from a reservoir outside the brain to specific targets inside the brain. This adds a new dimension to the 30-year-old process of injecting therapeutics into the brain through convection-enhanced delivery (CED), which uses continuous pressure over time to inject a fluid containing therapeutics into the brain. Because CED follows the path of least resistance, therapeutics don’t always hit the target.
Introducing an electrical field to the process — called electrokinetic convection-enhanced delivery or ECED — gives surgeons the power to design the delivery path and potentially cover brain lesions and tumors better.
“Delivering therapeutics by way of ECED has many applications,” explained Dr. Amir Faraji, principal investigator and Houston Methodist neurosurgeon. “It has the potential to improve gene therapy and tumor treatment, as well as treatment for traumatic brain injury and degenerative diseases — any number of situations where we need to get vital treatments to the brain in a more targeted manner.”
Delivering the correct dosage of drugs to the right place in the brain has long been a challenge. The same natural blood-brain barrier that protects our brains from toxins and pathogens can also block delivery of important medical treatments. Further research is needed before Faraji and team can bring this investigational therapy to humans.
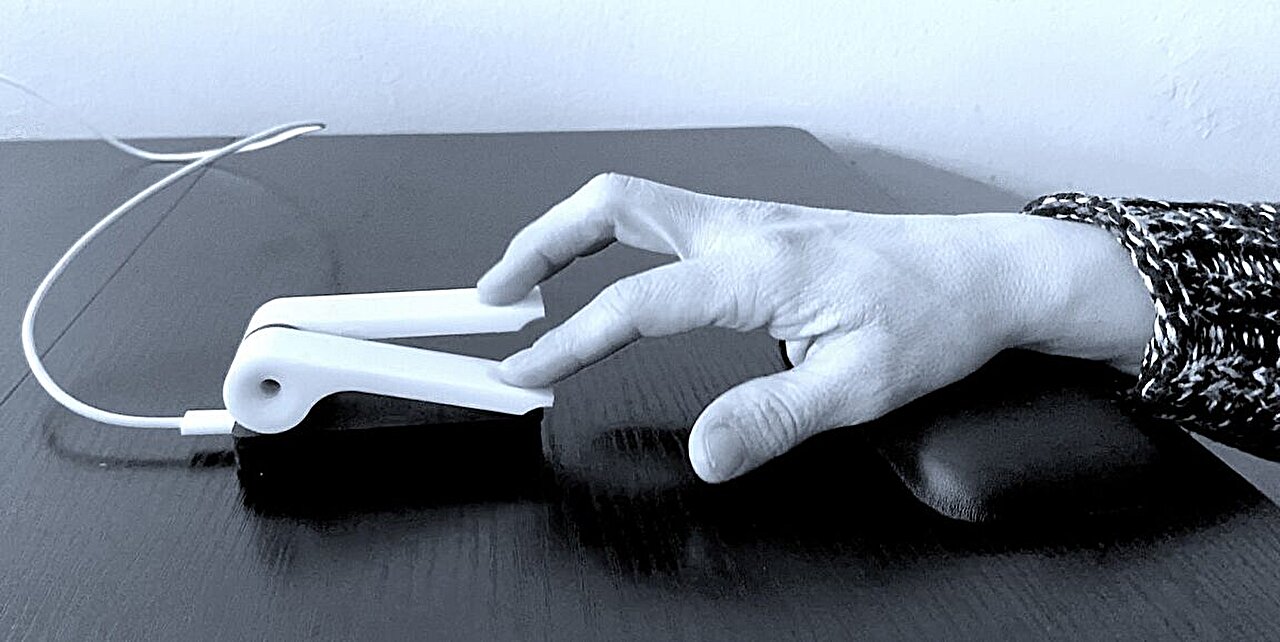
A “Behind the Paper” blog on the study — by Houston Methodist research scientist and co-author Jesus G. Cruz-Garza — explains how ECED can infuse macromolecules into the brain from a hydrogel reservoir placed at the brain’s surface.
“The brain acts as a charged porous scaffold that, in the presence of an electric field, allows for electroosmosis: bulk fluid flow in a porous media.” From the hydrogel reservoir, Cruz-Garza explains, this bulk flow of fluid enables the delivery of therapeutic agents.
This project was supported by the Houston Methodist Foundation and the Houston Methodist Research Institute Clinician-Scientist Award. It also received philanthropic funding from Paula and Rusty Walter and Walter Oil & Gas Corp Endowment at Houston Methodist: the John S. “Steve” Dunn, Jr. & Dagmar Dunn Pickens Gipe Chair in Brain Tumor Research; and grant number RP190587 from the Cancer Prevention and Research Initiative (CPRIT). Conducted at Houston Methodist Department of Neurosurgery, Houston Methodist Research Institute, Center for Neural Systems Restoration, Center for Neuroregeneration, in conjunction with Texas A&M University College of Medicine and School of Engineering.