Kids born in 2020 worldwide will experience twice the number of wildfires during their lifetimes compared with those born in 1960. In California and other western states, frequent wildfires have become as much a part of summer and fall as popsicles and Halloween candy.
Wildfires produce fine particulate matter, or PM₂.₅, that chokes the air and penetrates deep into lungs. Researchers know that short-term exposure to wildfire PM₂.₅ increases acute care visits for cardiorespiratory problems such as asthma. However, the long-term effects of repeated exposure to wildfire PM₂.₅ on chronic health conditions are unclear.
One reason is that scientists have not decided how best to measure this type of intermittent yet ongoing exposure. Environmental epidemiologists and health scientists like us usually summarize long-term exposure to total PM₂.₅ – which comes from power plants, industry and transportation – as average exposure over a year. This might not make sense when measuring exposure to wildfire. Unlike traffic-related air pollution, for example, levels of wildfire PM₂.₅ vary a lot throughout the year.
To improve health and equity research, our team has developed five metrics that better capture long-term exposure to wildfire PM₂.₅.
Measuring fluctuating wildfire PM₂.₅
To understand why current measurements of wildfire PM₂.₅ aren’t adequately capturing an individual’s long-term exposure, we need to delve into the concept of averages.
Say the mean level of PM₂.₅ over a year was 1 microgram per cubic meter. A person could experience that exposure as 1 microgram per cubic meter every day for 365 days, or as 365 micrograms per cubic meter on a single day.
While these two scenarios result in the same average exposure over a year, they might have very different biological effects. The body might be able to fend off damage from exposure to 1 microgram per cubic meter each day, but be overwhelmed by a huge, single dose of 365 micrograms per cubic meter.
For perspective, in 2022, Americans experienced an average total PM₂.₅ exposure of 7.8 micrograms per cubic meter. Researchers estimated that in the 35 states that experience wildfires, these wildfires added on average just 0.69 micrograms per cubic meter to total PM₂.₅ each year from 2016 to 2020. This perspective misses the mark, however.
For example, a census tract close to the 2018 Camp Fire experienced an average wildfire PM₂.₅ concentration of 1.2 micrograms per cubic meter between 2006 to 2020. But the actual fire event had a peak exposure of 310 micrograms per cubic meter – the world’s highest level that day.

Angela Weiss/AFP via Getty Images
Scientists want to better understand what such extreme exposures mean for long-term human health. Prior studies on long-term wildfire PM₂.₅ exposure focused mostly on people living close to a large fire, following up years later to check on their health status. This misses any new exposures that took place between baseline and follow-up.
More recent studies have tracked long-term exposure to wildfire PM₂.₅ that changes over time. For example, researchers reported associations between wildfire PM₂.₅ exposure over two years and risk of death from cancer and any other cause in Brazil. This work again relied on long-term average exposure and did not directly capture extreme exposures from intermittent wildfire events. Because the study did not evaluate it, we do not know whether a specific pattern of long-term wildfire PM₂.₅ exposure was worse for health.
Most days, people experience no wildfire PM₂.₅ exposure. Some days, wildfire exposure is intense. As of now, we do not know whether a few very bad days or many slightly bad days are riskier for health.
A new framework
How can we get more realistic estimates that capture the huge peaks in PM₂.₅ levels that people are exposed to during wildfires?
When thinking about the wildfire PM₂.₅ that people experience, exposure scientists – researchers who study contact between humans and harmful agents in the environment – consider frequency, duration and intensity. These interlocking factors help describe the body’s true exposure during a wildfire event.
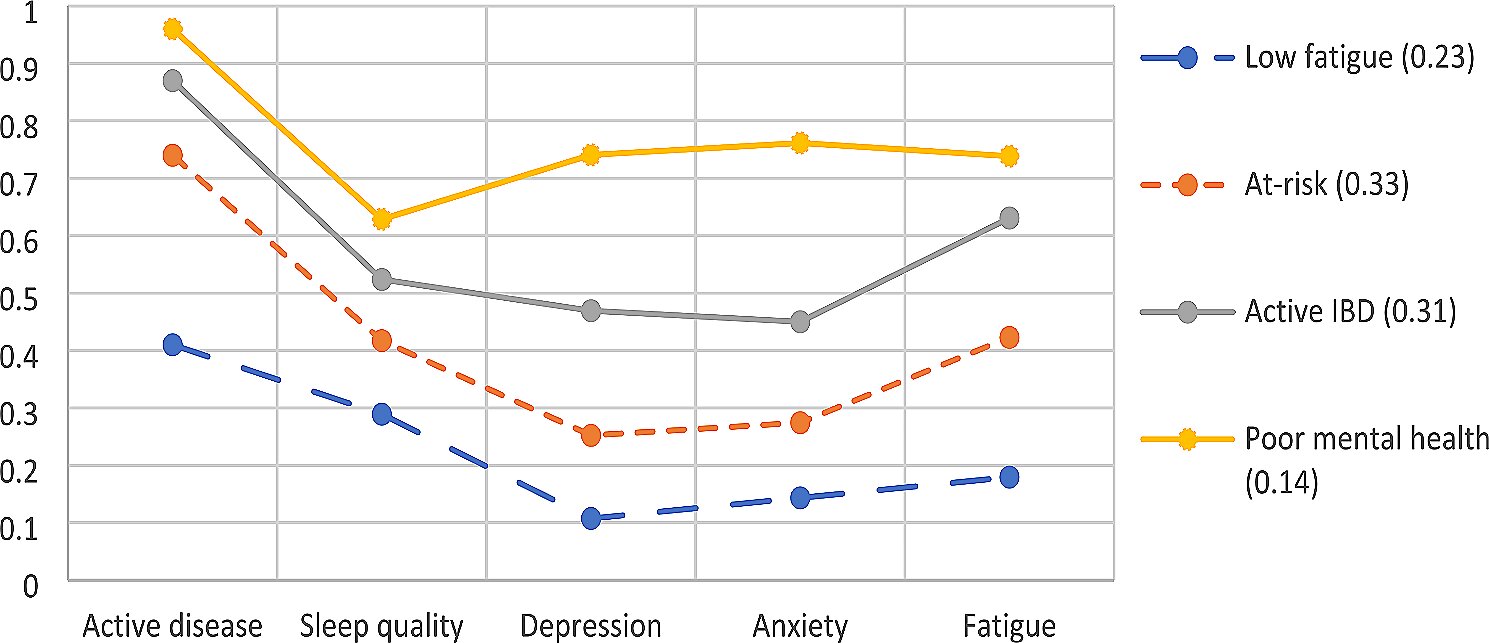
In our recent study, our team proposed a framework for measuring long-term exposure to wildfire PM₂.₅ that incorporates the frequency, duration and intensity of wildfire events. We applied air quality models to California wildfire data from 2006 to 2020, deriving new metrics that capture a range of exposure types.
Casey et al. 2024/PNAS, CC BY-NC-ND
One metric we devised is number of days with any wildfire PM₂.₅ exposure over a long-term period, which can identify even the smallest exposures. Another metric is average concentration of wildfire PM₂.₅ during the peak week of smoke levels over a long period, which highlights locations that experience the most extreme exposures. We also developed several other metrics that may be more useful, depending on what effects are being studied.
Interestingly, these metrics were quite correlated with one another, suggesting places with many days of at least some wildfire PM₂.₅ also had the highest levels overall. Although this can make it difficult to decide between different exposure patterns, the suitability of each metric depends in part on what health effects we are investigating.
Environmental injustice
We also assessed whether certain racial and ethnic groups experienced higher-than-average wildfire PM₂.₅ exposure and found that different groups faced the most exposure depending on the year.
Consider 2018 and 2020, two major wildfire years in California. The most exposed census tracts, by all metrics, were composed primarily of non-Hispanic white individuals in 2018 and Hispanic individuals in 2020. This makes sense, since non-Hispanic white people constitute about 41.6% and Hispanic people 36.4% of California’s population.
To understand whether other groups faced excess wildfire PM₂.₅ exposure, we used relative comparisons. This means we compared the true wildfire PM₂.₅ exposure experienced by each racial and ethnic group with what we would have expected if they were exposed to the state average.
We found that Indigenous communities had the most disproportionate exposure, experiencing 1.68 times more PM₂.₅ than expected. In comparison, non-Hispanic white Californians were 1.13 times more exposed to PM₂.₅ than expected, and multiracial Californians 1.09 times more exposed than expected.

Eric Thayer/Stringer via Getty Images News
Rural tribal lands had the highest mean wildfire PM₂.₅ concentrations – 0.83 micrograms per cubic meter – of any census tract in our study. A large portion of Native American people in California live in rural areas, often with higher wildfire risk due to decades of poor forestry management, including legal suppression of cultural burning practices that studies have shown to aid in reducing catastrophic wildfires. Recent state legislation has removed liability risks of cultural burning on Indigenous lands in California.
Understanding the drivers and health effects of high long-term exposure to wildfire PM₂.₅ among Native American and Alaska Native people can help address substantial health disparities between these groups and other Americans.