Late-life depression, typically defined as depression with onset in individuals over 60 years of age, can affect up to a third or more of people older than 60 and can be debilitating. But, like other neurological conditions, an individual’s risk may be influenced by lifestyle choices. Researchers from Mass General Brigham previously developed and validated the Brain Care Score (BCS) for helping patients and clinicians identify lifestyle changes that may reduce their risk of dementia and stroke. Now, with collaborators at Yale University, they have shown that a higher BCS is also associated with a lower risk of late-life depression. Findings, published in Frontiers in Psychiatry, provide further evidence of shared biological risk factors for stroke, dementia and depression and highlight the potential of the BCS to help patients make lifestyle changes to better care for their brain health.
“The Brain Care Score is a simple tool designed to help anyone in the world answer the question, ‘What can I do to take better care of my brain?'” said author Jonathan Rosand MD, MSc, co-founder of the McCance Center for Brain Health at Massachusetts General Hospital and the lead developer of the Brain Care Score. “This paper provides compelling evidence that raising your BCS is not only likely to make your brain healthier and more resistant to diseases like dementia and stroke, but that it also offers the hope of protection from depression.”
The new study represents a collaboration among researchers at Brigham and Women’s Hospital and Massachusetts General Hospital, founding members of the Mass General Brigham healthcare system.
“Dementia, stroke, and depression are leading causes of human suffering as we age,” said corresponding author Christopher D. Anderson, MD, MSc, chief of stroke and cerebrovascular diseases in the Department of Neurology at BWH. “This study highlights an extraordinary opportunity to prevent these conditions from developing in the first place.”
The Brain Care Score was developed by researchers at the McCance Center and their collaborators to help patients and clinicians prevent the onset of brain disease by focusing on modifiable risk factors. These include four physical risk factors (blood pressure, hemoglobin A1c, cholesterol and body mass index), five lifestyle elements (nutrition, alcohol intake, smoking, physical activity and sleep) and three social/emotional elements (stress, relationships and life purpose). A higher score on the 21-point scale is indicative of a lower risk of brain disease.
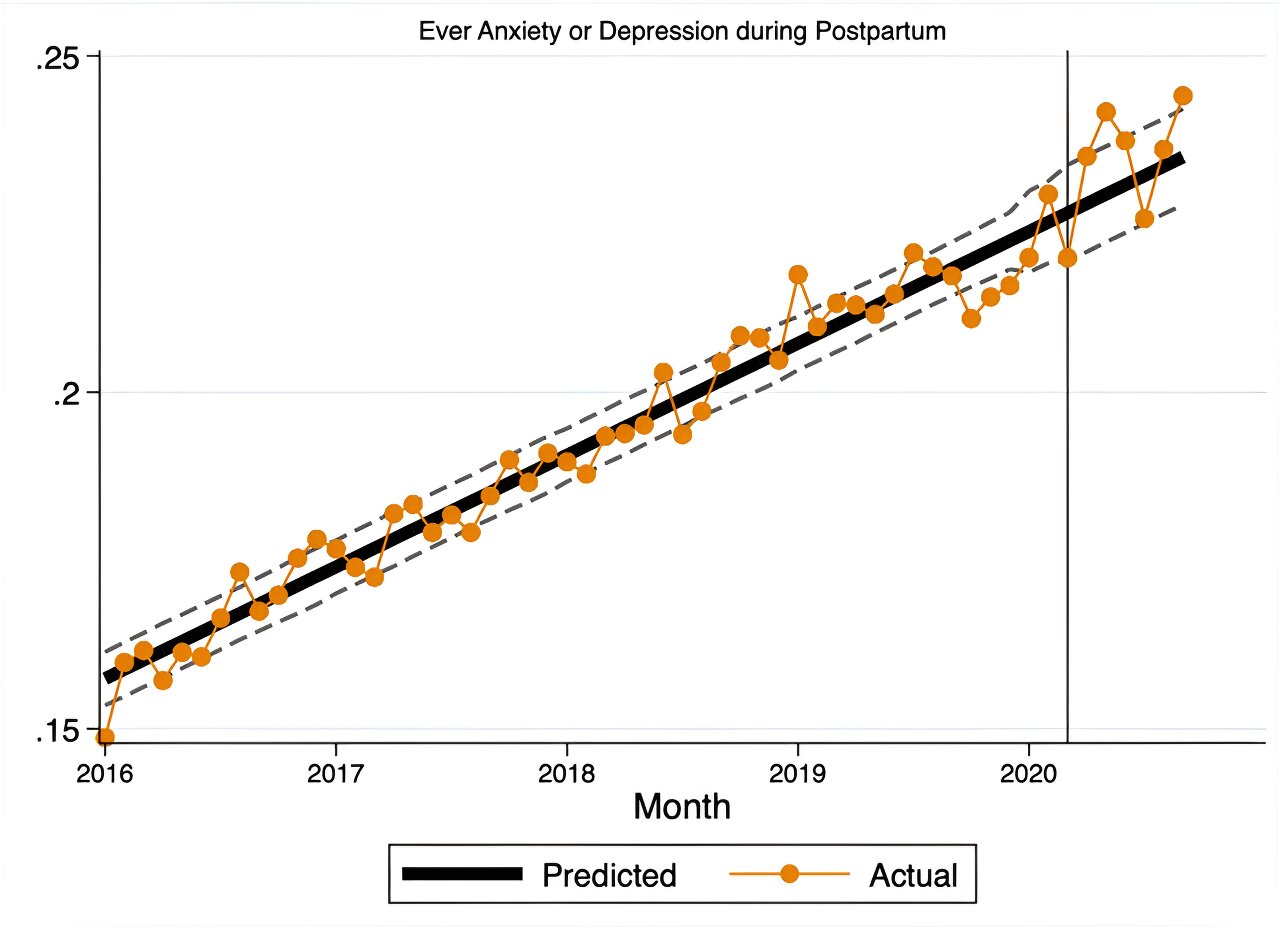
The research team, utilizing data from over 350,000 participants in the U.K. Biobank (UKB) study, demonstrated that a five-point increase in baseline BCS was associated with a 33 percent lower risk of late-life depression and a 27 percent lower composite risk of late-life depression, stroke and dementia over a median follow-up period of 13 years.
The UKB, which the researchers previously utilized to develop and validate the BCS, includes over a decade of systematically collected health information from participants throughout the U.K., who were 40-69 years old during the study’s enrollment period from 2006-2010. Additionally, the researchers verified their findings in a separate dataset of nearly 200,000 individuals from the UKB, whose primary care records were also accessible to the researchers. Under-diagnosis and under-documentation of depression is a known challenge to epidemiological research, but the inclusion of primary care records can reduce the likelihood of missing diagnoses.
When stratifying results by age, the researchers were surprised to find a substantial association between baseline BCS and risk of depression in those under 50 years of age. While the investigators expected that older individuals may experience neurodegenerative and inflammatory processes that can contribute to late-life depression, stroke and dementia, the neurobiological changes that lead to depression in younger individuals are less apparent. Going forward, the researchers are pursuing additional work to understand the relationship between BCS scores and risk of depression in the young.
“There is still much to be learned about what pathways contribute to late-life depression, dementia and stroke,” said first author Sanjula Singh, MD, PhD, MSc, of the McCance Center for Brain Health at Department of Neurology of Massachusetts General Hospital and Harvard Medical School. “Our results emphasize the importance of a holistic view of the brain to further understand underlying connections between different brain diseases.”
The investigators are pursuing ongoing research to determine whether individuals who increase their BSC over time by five points or more have a reduced risk of stroke and dementia in the future, compared to those without substantial score increases.
“Increasingly, data suggest that the risk for a variety of non-communicable diseases is to some extent mediated by modifiable lifestyle changes, should they be undertaken early enough,” said Gregory Fricchione, MD, associate chief of psychiatry at Massachusetts General Hospital. “This research is provocative and hopeful in its implications for tackling prevalent illnesses like depression, which itself is a risk factor for many other diseases. This research reminds us of the interlocking of the nervous system with psychosocial and immunological stress, along with the opportunity to reduce vulnerabilities to downstream damage to the brain through improvements in the factors outlined in the BCS.”
Authorship: Additional Mass General Brigham authors include Zeina Chemali (MGH), Leidys Gutierrez-Martinez (MGH), Livia Parodi (BWH, MGH), Ernst Mayerhofer (BWH, MGH), Jasper Senff (MGH), Courtney Nunley (MGH), Amy Newhouse (MGH), An Ouyang (MGH), M. Brandon Westover (MGH), Rudolph E. Tanzi (MGH), Bart Brouwers (MGH), Nirupama Yechoor (MGH), Christopher D. Anderson (BWH, MGH). Additional authors include Cyprien A. Rivier, Keren Papier, Santiago Clocchiatti-Tuozzo, Ronald M. Lazar, Aleksandra Pikula, Sarah Ibrahim, Virginia Howard, George Howard, Thomas Littlejohns, Kevin N. Sheth, Guido J. Falcone.
Disclosures: Rosand receives sponsored research support from the U.S. National Institutes of Health and the American Heart Association and receives payments for expert testimony and consulting fees from the National Football League. A complete list of disclosures is included in the paper.
Funding: Funding provided by the Lavine Brain Health Innovation Fund and the McCance Center for Brain Health. A complete list of additional research support is included in the article.