A new study helps explain why having ApoE4—the gene variant most closely linked to Alzheimer’s disease—increases the risk of neurodegeneration and white matter damage.
Researchers at Weill Cornell Medicine discovered that immune cells in the brain called border-associated macrophages (BAMs) are a source of ApoE4 protein and contribute to damaging blood vessels and brain tissue.
The study, published in Nature Neuroscience, may help scientists identify new approaches to preventing or treating Alzheimer’s disease in people who carry the ApoE4 gene and other forms of age-related brain disease.
The APOE gene encodes apolipoprotein E (ApoE), which has many roles in the brain. It also has several common variants (ApoE2, ApoE3 and ApoE4), of which ApoE4 increases the risk for Alzheimer’s disease up to 12-fold. ApoE4 also increases the risk of damage to the white matter that underlies vascular dementia, the second-most common cause of cognitive impairment after Alzheimer’s disease. However, how ApoE4 produces these damaging effects on the brain is not completely clear.
“Our study points to border-associated macrophages as a critical mediator of these deleterious effects and helps us understand how ApoE4 may contribute to damaging blood vessels and brain white matter in patients with Alzheimer’s disease or other forms of age-related brain disease,” said the study’s co-senior author, Laibaik Park, associate professor of research in neuroscience at the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine.
“We previously showed in another model that the amyloid beta protein that builds up in the brains of patients with Alzheimer’s disease interacts with a protein receptor on BAMs,” said Antoine Anfray, instructor in neuroscience at the Brain and Mind Research Institute, and first author of the study. This triggers a chain reaction that damages blood vessels, preventing them from clearing amyloid, which leads to degeneration of brain tissue.
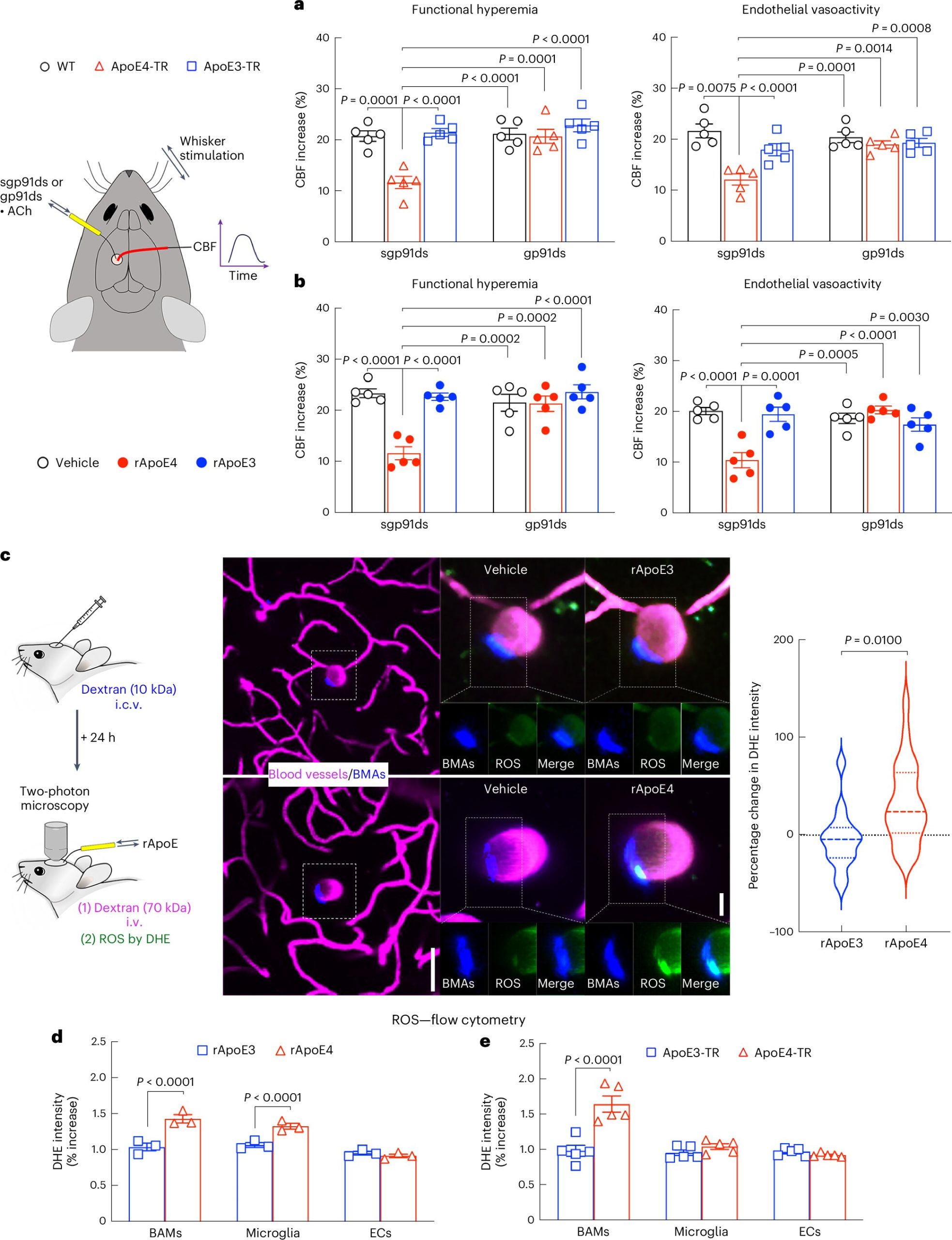
In their latest study, the researchers show that pre-clinical models genetically engineered to express the human ApoE4 variant developed impaired blood vessels and tissue damage in their brains, while those with the more benign ApoE3 remain healthy. They found that BAMs with the ApoE4 variant produce inflammatory oxygen free radicals, which damage the blood vessels. As a result, blood flow needed to remove waste and repair damage to the brain tissue is limited.
Surprisingly, when the animal models with the ApoE4 variant had their BAMs removed, they didn’t experience this damaging cascade. The study also showed that the BAMs are not only the mediators of the damage induced by ApoE4, but also the source of ApoE4 causing the damage. Accordingly, reducing ApoE4 expression in BAMs eliminated the harmful vascular effects.
“These findings show BAMs are both the source and the target of the ApoE4 necessary for damage to blood vessels,” said study senior author Dr. Costantino Iadecola, director and chair of the Brain and Mind Research Institute and the Anne Parrish Titzell Professor of Neurology at Weill Cornell Medicine.
The investigators further confirmed that ApoE4 and BAMs transferred to animal models which didn’t have the ApoE4 variant developed blood vessel and tissue damage. Alternatively, transplanting BAMs from animals with the ApoE3 variant to animals with the ApoE4 variant reversed the damage.
The findings may help explain why some patients are more likely to experience harmful swelling and bleeding in the brain when treated with amyloid-removing antibody drugs like Lecanemab, a complication most frequent in patients with ApoE4. This complication, termed amyloid related imaging abnormality (ARIA), requires the treatment to be stopped, limiting its benefits in slowing the progression of early-stage Alzheimer’s disease.
Understanding how blood vessels are more vulnerable in some patients may help scientists develop ways to prevent this adverse effect by suppressing ApoE4 production by BAMs. Iadecola and Park are working on developing such interventions, but they caution that more work is needed before the findings can be applied in the clinic.
For now, they are looking for ways to block the receptors that mediate ApoE4-related blood vessel damage to reduce or prevent the genetic variant’s harmful effects on the amyloid-beta clearance pathway.
“We now know that ApoE4 from border-associated macrophages increases blood vessel damage, but the next step would be to actually find a way to target the macrophages to enhance amyloid and tau clearance,” Iadecola said. “Can genetically switching the ApoE4 to the ApoE3 genetic variant remove amyloid build up better? That will be proof-of-concept.”
More information:
Anfray, A et al, A cell-autonomous role for border-associated macrophages in ApoE4 neurovascular dysfunction and susceptibility to white matter injury. Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01757-6. www.nature.com/articles/s41593-024-01757-6
Citation:
Immune cells linked to blood vessel damage and neurodegeneration (2024, September 19)
retrieved 7 October 2024
from https://medicalxpress.com/news/2024-09-immune-cells-linked-blood-vessel.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.