For years, cancer researchers have noticed that more men than women get a lethal form of brain cancer called glioblastoma. They’ve also found that these tumors are often more aggressive in men. But pinpointing the characteristics that might help doctors forecast which tumors are likely to grow more quickly has proven elusive. University of Wisconsin–Madison researchers are turning to artificial intelligence to reveal those risk factors and how they differ between the sexes.
Radiology and biomedical engineering professor Pallavi Tiwari and her colleagues have published their initial findings in the journal Science Advances, hinting at the promise of AI for improving medical care for cancer patients.
“There’s a ton of data collected in a cancer patient’s journey,” says Tiwari, who is also affiliated with the department of medical physics. “Right now, unfortunately, it’s usually studied in a siloed fashion, and this is where AI has huge potential.”
Few researchers better understand this potential than Tiwari. Arriving at UW–Madison in 2022 to help lead the university’s new AI initiative in medical imaging, Tiwari co-directs the Imaging and Radiation Sciences Program at the Carbone Cancer Center. Her research leverages the computational power of AI models to probe large volumes of medical images and find patterns that could help oncologists and their patients make better-informed decisions.
“We want to address the entire spectrum of challenges in a cancer patient’s journey, starting from diagnosis and prognosis to treatment response assessment,” says Tiwari.
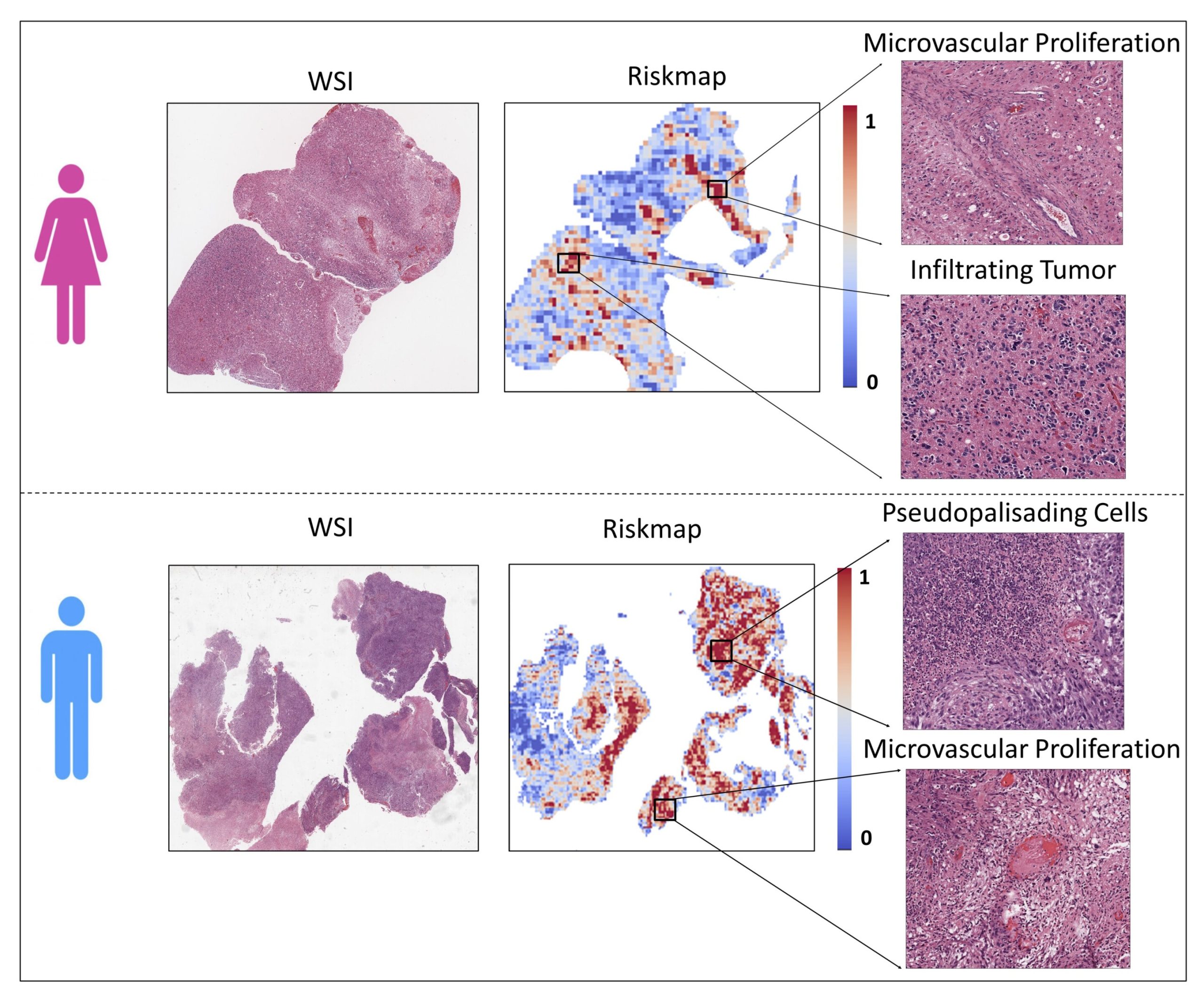
In this case, Tiwari and former graduate student Ruchika Verma turned to digital images of pathology slides—thin slices of tumor samples—in search of patterns that might forecast how quickly a tumor could grow and thus how long a patient might expect to survive.
Glioblastoma is one of the most aggressive forms of cancer, with a median survival of 15 months after diagnosis.
“Patients often don’t have long lives after diagnosis,” says Tiwari. “But a big challenge is prognosis—identifying how long patients are actually going to live and what their outcome is likely to be. This is important because the outcomes ultimately govern the treatments that they’re getting and their quality of life after diagnosis.”
To tackle this challenge, Tiwari and Verma built an AI model that can identify even subtle patterns in pathology slides that might never be apparent to the naked eye. Using data from more than 250 studies of glioblastoma patients, they trained the model to recognize tumors’ unique characteristics, such as the abundance of certain cell types and the degree to which they invade surrounding healthy tissue.
Further, they trained the model to identify any patterns between these characteristics and patients’ survival time while accounting for their sex.
In doing so, they developed an AI model that was able to identify risk factors for more aggressive tumors that are strongly associated with each sex. For females, higher-risk characteristics included tumors that were infiltrating into healthy tissue. Among males, the presence of certain cells that surround dying tissue (called pseudopalisading cells) was associated with more aggressive tumors.
The model also identified tumor characteristics that appear to translate to worse prognoses for both men and women.
The study could help lead to more individualized care for glioblastoma patients.
“By uncovering these unique patterns, we hope to inspire new avenues for personalized treatment and encourage continued inquiry into the underlying biological differences seen in these tumors,” Verma says.
Tiwari and her colleagues are doing similar work using MRI data and have begun using AI to analyze pancreatic and breast cancers with the aim of improving outcomes for patients.
In addition to her research, Tiwari is helping to shape the university’s RISE-AI and RISE-THRIVE initiatives, which are establishing UW–Madison as a leader of cross-disciplinary research on artificial intelligence and the human health span, respectively.
“UW has a rich and diverse expertise across our engineering and medical campuses,” says Tiwari, “and with the RISE initiatives, we are well positioned to be at the forefront of translating AI research in clinical care.”
More information:
Ruchika Verma et al, Sexually dimorphic computational histopathological signatures prognostic of overall survival in high-grade gliomas via deep learning, Science Advances (2024). DOI: 10.1126/sciadv.adi0302
Citation:
AI model shows potential for identifying sex-specific risks associated with brain tumors (2024, October 7)
retrieved 7 October 2024
from https://medicalxpress.com/news/2024-10-ai-potential-sex-specific-brain.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.