A new study finds that preschool-aged children with sickle cell disease (SCD) who live in food deserts and have limited access to transportation are at greater risk for acute complications and hospitalizations, despite receiving free evidence-based therapy and social support, according to results published in Blood Advances.
“Despite the level of care received by the families and patients within our clinic, we still have a gap in terms of being able to address the barriers they’re experiencing within the community,” said senior study author Jason Hodges, Ph.D., MA, director of research and clinical studies in the Department of Hematology at St. Jude’s Children’s Research Hospital in Memphis.
“We need to think about the neighborhood and context that these patients and families are coming from because that has a huge impact on health.”
While previous studies have shown that social determinants of health (SDoH)—the conditions in which people are born, grow, work, live, and learn—can impact the health of children with SCD, less is known about how community-level factors, such as transportation access, income level, education attainment, and proximity to a grocery store may contribute to health disparities in these patients.
For this study, Dr. Hodges and his team wanted to take a more granular look at specific community-level SDoH—for example, household distance from grocery stores, number of children in the household, vehicle ownership, neighborhood income, and parental education levels—to assess whether these factors are associated with increased acute care utilization (ACU), including emergency department visits and hospitalizations, among preschool-aged children with SCD.
The researchers analyzed demographic, treatment, and ACU data for 435 children ages 0-6 years (median of 5.7 years) enrolled in the Sickle Cell Disease Clinical Research and Intervention Program, a longitudinal study evaluating the treatment, health care use, and outcomes of individuals living with SCD throughout their lifespan.
Participants’ home addresses were mapped and grouped by census tract and compared with census-level data on household poverty levels and food access from the U.S. Department of Agriculture Food Access Research Atlas.
All participants were Black. Half (52%) were female, and just over half (60%) of participants had the severe SCD genotype (HbSS/HbSb0thalassemia). Some 43% of the patients resided in neighborhoods identified by the U.S. Census as being particularly vulnerable to hardship.
All participants were receiving the standard of care, hydroxyurea and/or monthly transfusions when needed, as well as social support, including transportation and meal services when they came for their appointments.
After controlling for sickle SCD genotype and disease-modifying therapy, the team found that living in a household located more than one mile from a supermarket was associated with a 44% increase in hospitalizations and a 37% increase in ACU among children with SCD ages 0–6 years.
Living in a household more than a mile from a grocery store and without a vehicle was associated with a significantly higher likelihood of being hospitalized before age six. Conversely, in households with an adult holding at least one bachelor’s degree (11.7%), children with SCD were 33% less likely to experience ACU and hospitalizations respectively, suggesting parental education level could have a protective effect.
“The data suggest that, regardless of how much care you provide and how many new therapies are out there for patients who have chronic illnesses like SCD, unless you start addressing these deep-rooted issues, like food deserts or quality of life from the neighborhood standpoint, it’s always going to be extremely tricky to holistically provide care to our patient population,” said lead study author Hamda Khan, MA, a clinical research associate in the Department of Hematology at St. Jude’s Children’s Research Hospital.
Khan and Dr. Hodges hope these data about the impact of neighborhoods and other community-level SDoH on the health of patients with SCD will help shape public policy to bring more resources and public health interventions to these high-need areas.
They say further research should focus on household size, health care maintenance visits, and environmental hazards like air pollution to better understand the impact of environmental SDoH on this patient population.
The authors cautioned that this research is specific to children with SCD ages 0–6 years who received wrap-around care and social support and may not reflect the experience of older patients with SCD, patients who have relocated to areas with better access to resources, or those not receiving support services. Additional limitations may include insufficient data on adherence to disease-modifying therapy.
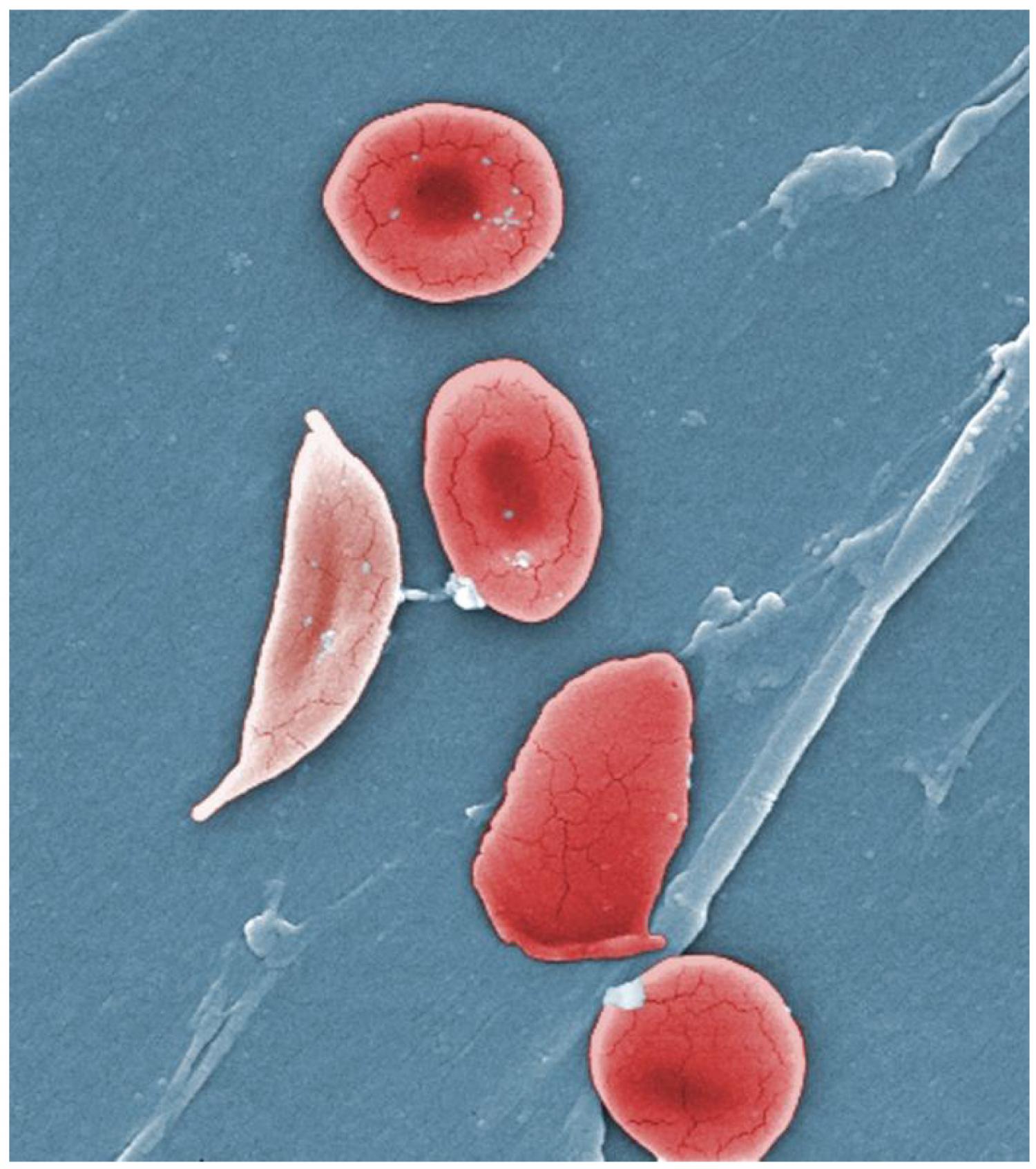
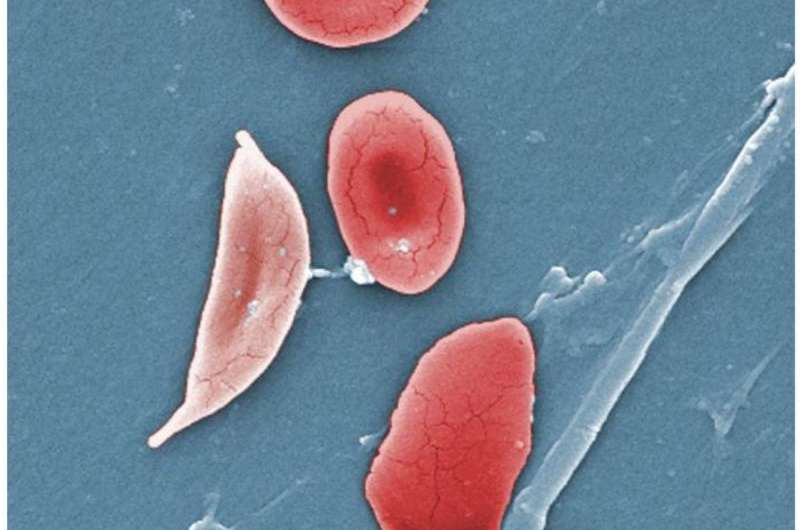
SCD is the most common inherited blood cell disorder in the United States, affecting an estimated 100,000 people and one out of every 365 Black or African American births. SCD is characterized by misshapen red blood cells that can block blood vessels, causing episodes of severe pain, as well as damage to tissues and organs.
More information:
Blood Advances (2024).
Citation:
Food deserts, limited access to transportation linked to more complications among preschoolers with sickle cell disease (2024, October 7)
retrieved 7 October 2024
from https://medicalxpress.com/news/2024-10-food-limited-access-linked-complications.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.