An estimated one in five Americans live with chronic pain and current treatment options leave much to be desired. Feixiong Cheng, Ph.D., Director of Cleveland Clinic’s Genome Center, and IBM are using artificial intelligence (AI) for drug discovery in advanced pain management. The team’s deep-learning framework identified multiple gut microbiome-derived metabolites and FDA-approved drugs that can be repurposed to select non-addictive, non-opioid options to treat chronic pain.
The findings, published in Cell Press, represent one of many ways the organizations’ Discovery Accelerator partnership is helping to advance research in healthcare and life sciences.
Treating chronic pain with opioids is still a challenge due to the risk of severe side effects and dependency, says co-first author Yunguang Qiu, Ph.D., a postdoctoral fellow in Dr. Cheng’s lab whose research program focuses on developing therapeutics for nervous system disorders. Recent evidence has shown that drugging a specific subset of pain receptors in a protein class called G protein-coupled receptors (GPCRs) can provide non-addictive, non-opioid pain relief. The question is how to target those receptors, Dr. Qiu explains.
Instead of inventing new molecules from scratch, the team wondered whether they could apply research methods they had already developed for finding preexisting FDA-approved drugs for potential pain indication. Part of this process involves mapping out gut metabolites to spot drug targets.
To identify these molecules, the first author and computational scientist Yuxin Yang, Ph.D., a former Kent State University graduate student. Dr. Yang completed his thesis research in Dr. Cheng’s lab and continues to work there as a data scientist. Drs. Yang and Qiu led a team to update a previous drug discovery AI algorithm the Cheng Lab had developed. Collaborators from IBM helped write and edit the manuscript.
“Our IBM collaborators gave us valuable advice and perspective to develop advanced computational techniques,” Dr. Yang says. “I’m happy for the opportunity to work with and learn from peers in the industry sector.”
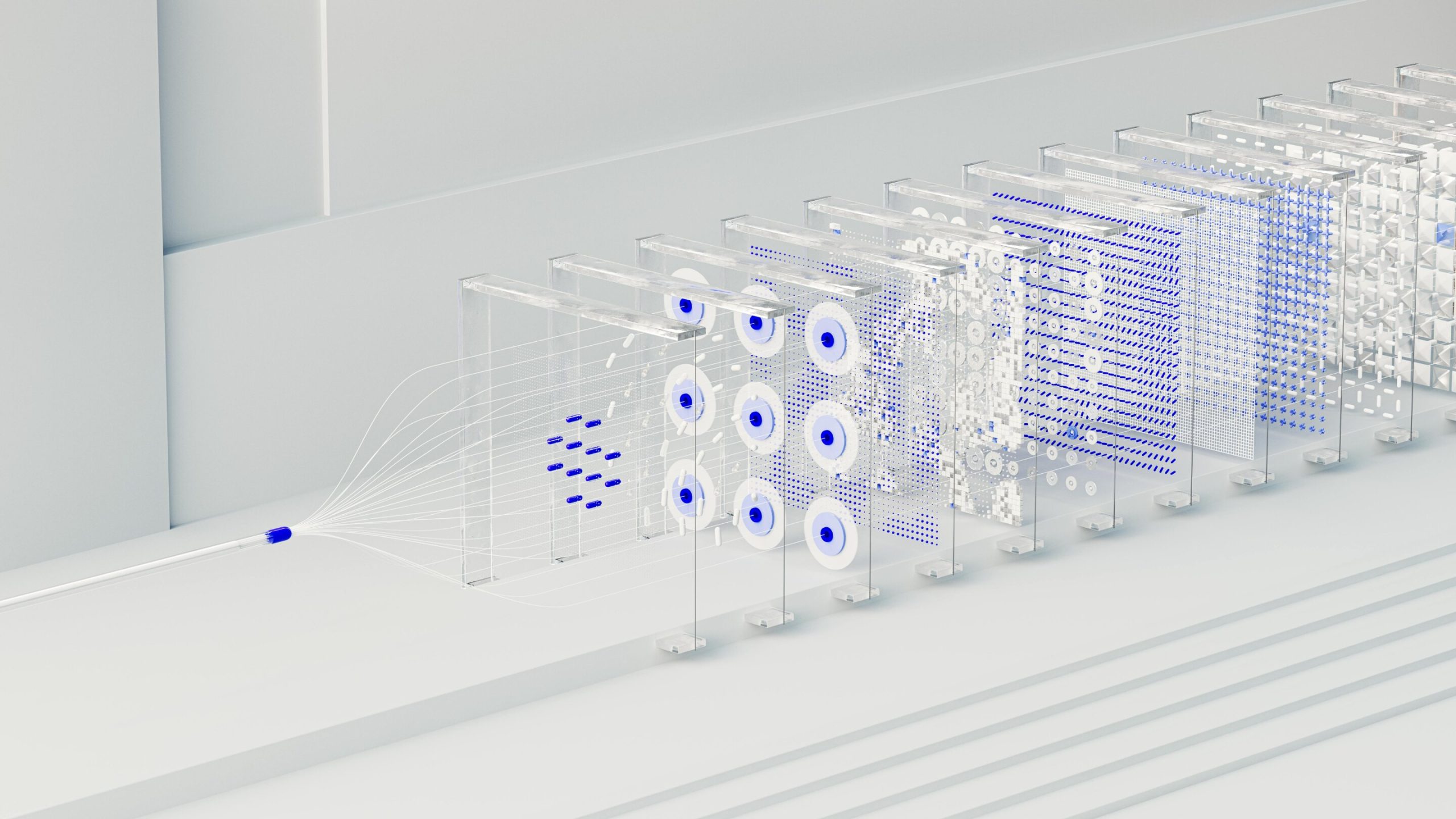
To determine whether a molecule will work as a drug, researchers need to predict how it will physically interact with and influence proteins in our body (in this case, our pain receptors). To do this, the researchers need a 3D understanding of both molecules based on extensive 2D data about their physical, structural and chemical properties.
“Even with the help of current computational methods, combining the amount of data we need for our predictive analyses is extremely complex and time-consuming,” Dr. Cheng explains. “AI can rapidly make full use of both compound and protein data gained from imaging, evolutionary and chemical experiments to predict which compound has the best chance of influencing our pain receptors in the right way.”
The research team’s tool, called LISA-CPI (Ligand Image- and receptor’s three-dimensional (3D) Structures-Aware framework to predict Compound-Protein Interactions) uses a form of artificial intelligence called deep learning to predict:
- if a molecule can bind to a specific pain receptor
- where on the receptor a molecule will physically attach
- how strongly the molecule will attach to that receptor
- whether binding a molecule to a receptor will turn signaling effects turn on or off
The team used LISA-CPI to predict how 369 gut microbial metabolites and 2,308 FDA- approved drugs would interact with 13 pain-associated receptors. The AI framework identified several compounds that could be repurposed to treat pain. Studies are underway to validate these compounds in the lab.
“This algorithm’s predictions can lessen the experimental burden researchers must overcome to even come up with a list of candidate drugs for further testing,” Dr. Yang says. “We can use this tool to test even more drugs, metabolites, GPCRs and other receptors to find therapeutics that treat diseases beyond pain, like Alzheimer’s disease.”
Dr. Cheng added that this is just one example of how the team is collaborating with IBM to develop small molecule foundation models for drug development—including both drug repurposing in this study and an ongoing novel drug discovery project.
“We believe that these foundation models will offer powerful AI technologies to rapidly develop therapeutics for multiple challenging human health issues,” he says.
More information:
Yuxin Yang et al, A deep learning framework combining molecular image and protein structural representations identifies candidate drugs for pain, Cell Reports Methods (2024). DOI: 10.1016/j.crmeth.2024.100865
Citation:
Researchers use AI to find non-opioid pain relief options (2024, October 6)
retrieved 6 October 2024
from https://medicalxpress.com/news/2024-10-ai-opioid-pain-relief-options.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.